CPT® DEFINITION OF NEW VS. ESTABLISHED PATIENTS
The CPT® definition of a new patient underwent subtle changes in 2012. Unfortunately, CMS did not change their definition to stay aligned with these changes. This difference in language has caused great confusion for many qualified healthcare practitioners trying to stay compliant with the complex rules and regulations of E&M. I encourage all readers to have a handy copy of the American Medical Association's CPT® manual for quick and easy reference. The 2015 standard edition manual is available for purchase from Amazon by clicking on the image to the right. How does the 2014 CPT® manual define a new patient?
Let's look at this definition a little closer. The 2014 CPT® manual defines professional services as those face-to-face services provided by physicians or other qualified health care professionals who may report an E/M service by a specific CPT® code. In other words, if you provided a service, such as interpretation of an EKG or you read an echo, or you called in a prescription but you did not provide a billable E/M face-to-face encounter, the patient is still considered a new patient by the definition of professional services. The 2012 updated definition of a new patient also added in the the words exact as well as and subspecialty. Unfortunately, CMS did not change their definition to recognize this change in specialty determination.A new patient is one who has not received any professional services from the physician/qualified health care professional or another physician/qualified health care professional of the exact same specialty and subspecialty who belongs to the same group practice, within the past three years.
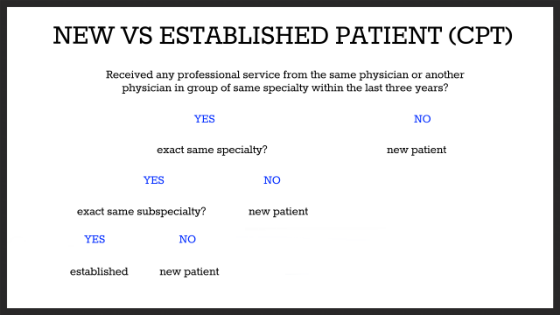
CPT® DEFINITION DECISION TREE
Decision trees may provide an easier way for qualified practitioners to understand these rules. A new vs. established patient decision tree analysis is provided here, as it is in the CPT® manual.
CMS DEFINITION OF NEW VS. ESTABLISHED PATIENTS
CMS provides insight into their definition of new versus established patients in several important resources. These definitions are not the same as the updated 2012 CPT® definition. First, a CMS definition of a new patient is provided in section 30.6.7 of Chapter 12 of the Medicare Claims Processing Manual (pdf page 52). From section A:
Definition of New Patient for Selection of E/M Visit Code
Interpret the phrase “new patient” to mean a patient who has not received any professional services, i.e., E/M service or other face-to-face service (e.g., surgical procedure) from the physician or physician group practice (same physician specialty) within the previous 3 years. For example, if a professional component of a previous procedure is billed in a 3 year time period, e.g., a lab interpretation is billed and no E/M service or other face-to-face service with the patient is performed, then this patient remains a new patient for the initial visit. An interpretation of a diagnostic test, reading an x-ray or EKG etc., in the absence of an E/M service or other face-to-face service with the patient does not affect the designation of a new patient.
For purposes of billing for E/M services, patients are identified as either new or established, depending on previous encounters with the provider.
A new patient is defined as an individual who has not received any professional services from the physician/non-physician practitioner (NPP) or another physician of the same specialty who belongs to the same group practice within the previous three years.
An established patient is an individual who has received professional services from the physician/NPP or another physician of the same specialty who belongs to the same group practice within the previous three years.Both definitions lack the updated CPT® definition that includes the exact same specialty and subspecialty. This has lead to great confusion when trying to define when a patient is new vs. established within the same group practice but of different specialty or subspecialty. For patients not covered by Medicare, knowing how the insurance carrier reconciles this difference may prevent delays or denials of claims.
DEFINITION OF A GROUP PRACTICE (CMS)
One must also know how to define a group practice to interpret the new and established patient rules. Medicare has defined a group practice in Chapter 5 of Medicare General Information, Eligibility, and Entitlement. Section 90.4 (pdf page 38) says:
A group practice is a group of two or more physicians and non-physician practitioners legally organized in a partnership, professional corporation, foundation, not-for-profit corporation, faculty practice plan, or similar association:
- In which each physician who is a member of the group provides substantially the full range of services which the physician routinely provides (including medical care, consultation, diagnosis, or treatment) through the joint use of shared office space, facilities, equipment, and personnel;
- For which substantially all of the services of the physicians who are members of the group are provided through the group and are billed in the name of the group and amounts so received are treated as receipts of the group;
- In which the overhead expenses of and the income from the practice are distributed in accordance with methods previously determined by members of the group; and
- Which meets such other standards as the Secretary may impose by regulation to implement §1877(h)(4) of the Social Security Act. The group practice definition also applies to health care practitioners.
This Medicare carrier further clarifies the definition of a group practice by stating we determine whether physicians are members of the same group based on the Tax Identification Number. They also have an assortment of other clinically relevant scenarios in question and answer format. I encourage all readers to review them for their own educational value.
RECOGNIZED MEDICARE SPECIALTIES
Physicians are allowed to choose a primary and a secondary specialty code. If the carrier and DMERC provider file can accommodate only one specialty code, the carrier or DMERC assigns the code that corresponds to the greater amount of allowed charges. For example, if the practice is 50 percent ophthalmology and 50 percent otolaryngology, the carrier/DMERC compares the total allowed charges for the previous year for ophthalmology and otolaryngology services. They assign the code that corresponds to the greater amount of the allowed charges.
- 01 General Practice
- 02 General Surgery
- 03 Allergy/Immunology
- 04 Otolaryngology
- 05 Anesthesiology
- 06 Cardiology
- 07 Dermatology
- 08 Family Practice
- 09 Interventional Pain Management
- 10 Gastroenterology
- 11 Internal Medicine
- 12 Osteopathic Manipulative Medicine
- 13 Neurology
- 14 Neurosurgery
- 16 Obstetrics/Gynecology
- 17 Hospice and Palliative Care
- 18 Ophthalmology
- 19 Oral Surgery (dentists only)
- 20 Orthopedic Surgery
- 21 Cardiac Electrophysiology
- 22 Pathology
- 23 Sports Medicine
- 24 Plastic and Reconstructive Surgery
- 25 Physical Medicine and Rehabilitation
- 26 Psychiatry
- 27 Geriatric Psychiatry
- 28 Colorectal Surgery (formerly proctology)
- 29 Pulmonary Disease
- 30 Diagnostic Radiology
- 33 Thoracic Surgery
- 34 Urology
- 35 Chiropractic
- 36 Nuclear Medicine
- 37 Pediatric Medicine
- 38 Geriatric Medicine
- 39 Nephrology
- 40 Hand Surgery
- 41 Optometry
- 44 Infectious Disease
- 46 Endocrinology
- 48 Podiatry
- 66 Rheumatology
- 70 Single or Multispecialty Clinic or Group Practice
- 72 Pain Management
- 73 Mass Immunization Roster Biller
- 76 Peripheral Vascular Disease
- 77 Vascular Surgery
- 78 Cardiac Surgery
- 79 Addiction Medicine
- 81 Critical Care (Intensivists)
- 82 Hematology
- 83 Hematology/Oncology
- 84 Preventative Medicine
- 85 Maxillofacial Surgery
- 86 Neuropsychiatry
- 90 Medical Oncology
- 91 Surgical Oncology
- 92 Radiation Oncology
- 93 Emergency Medicine
- 94 Interventional Radiology
- 98 Gynecological/Oncology
- 99 Unknown Physician Specialty
- C0 Sleep Medicine
RECOGNIZED AMA SPECIALTIES AND SUBSPECIALTIES
What about other specialties or subspecialties not recognized by Medicare? Here are several nice resources reviewing AMA physician specialty codes
- AMA physician specialty groups and codes
- American Medical Association self designated practice specialty definitions
- Side-by-side comparison AMA and Medicare recognized specialties.
DIFFERENCE BETWEEN CPT® AND CMS CAUSING CONFUSION
NEW VS. ESTABLISHED PATIENT DETERMINATION DOES NOT APPLY
By CPT® definition, not all E/M codes require the qualified practitioner to determine if the patient is new or established. Which common E/M code groups are excluded from the new patient vs. old patient determination?
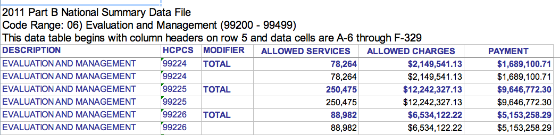
- Initial observation care (99218-99220)
- Subsequent observation care (99224-99226)
- Observation care discharge services (99217)
- Initial hospital care (99221-99223)
- Subsequent hospital care (99231-99233)
- Admission and Discharge Services same day (99234-99236)
- Hospital discharge services (99238, 99239)
- Critical care services (99291, 99292)
- Emergency department services (99281-99285)
- Initial nursing facility care (99304-99306)
- Subsequent nursing facility care (99307-99310)
- Inpatient consultations (99251-99255). This code group is no longer recognized by CMS.
- Office or other outpatient consultations (99241-99245). This code group is no longer recognized by CMS.
NEW VS. ESTABLISHED PATIENT DETERMINATION DOES APPLY
By CPT® definition, some E/M codes require the practitioner to determine whether the face-to-face encounter involves a new patient or an established patient.
- Office or other outpatient services new patient (99201-99205)
- Office or other outpatient services established patient (99211-99215)
- Domiciliary, rest home (eg, boarding home), or custodial care services new patient (99324-99328)
- Domiciliary, rest home (eg, boarding home), or custodial care services established patient (99334-99337)
- Home services new patient (99341-99345)
- Home services established patient (99347-99350)
- Preventative medicine services new patient (99381-99387)
- Preventative medicine services established patient (99391-99397)
NEW VS. ESTABLISHED CLINICAL EXAMPLES IN THE HOSPITAL
Most E/M code groups used in the hospital do not require the practitioner to determine whether the patient is new or established in their group practice. However, one common hospital billing and coding scenario does require quite a bit of effort to determine the correct E/M code group. As a consultant caring for a Medicare patient in the hospital under ambulatory surgery center (ASC) or observation status, practitioners are directed to use the office or other outpatient service codes. This also applies to any other patient who's insurance does not accept consultation codes. Determining whether the patient is a new patient or an established patient is necessary to prevent delays or denials in payment.
A 42 year old morbidly obese man with chronic lymphedema and a diagnosis of bilateral cellulitis is admitted to observation status by a hospitalist in a different group as a direct admission from the primary care physician's office with a request to consult an infectious disease specialist.In this scenario, the hospitalist would use the attending physician initial observation code group 99218-99220 for the admission, code group 99224-99226 for subsequent care visits and 99217 for the date of discharge. However, the infectious disease (ID) consultant would first have to know whether the patient's insurance carrier accepts consultation codes. If they do, the initial encounter should be coded as an outpatient consultation (99241-99245). All subsequent care visits should be coded as office or other outpatient services of an established patient (99211-99215).
However, if the patient's insurance does not accept consultation codes, then the ID consulting specialist must determine whether the patient is a new patient or an established patient in their group practice. If the ID specialist determines the patient is new, they should bill their initial encounter as an office or other outpatient service of a new patient using code group 99201-99205. If they determine the patient is an established patient of their group practice, they should choose the office or other outpatient service established patient code group 99211-99215 as their initial and all subsequent care visits. Here is another clinical example.
A healthy 37 year old with stable seasonal allergies is admitted under ASC status by an orthopedic surgeon for shoulder surgery. The hospitalist is consulted for medical management.What should the hospitalist bill? The hospitalist must follow the same decision analysis as the ID specialist did in the clinical example above. Most hospitalists do not have their own office charts or EMR to reference when trying to determine if they have seen the patient in the last three years. The only way to know for sure whether any other hospitalist or other physician of the same specialty or non-physician practitioner (NPP) working with the same specialty in the same group practice has seen the patient in the last three years is to search their hospital's EHR for evidence of any prior H&P, consult note or other face-to-face E/M progress note visit that would qualify as a professional service. Most doctors don't have the time, energy, education or resources to figure all that out.
NEW VS. ESTABLISHED CLINICAL EXAMPLE IN THE OFFICE
Excluding consultation codes, choosing new vs. established codes in the office is straight forward. Either the patient is or isn't a new patient based on the prevailing rules of the patient's third party payer. If the patient is a new patient, choose code group 99201-99205 for the initial encounter and 99211-99215 for subsequent established care visits until it is determined the patient is no longer an established patient. If the patient is not a new patient, established care codes should be used.
If consultation codes are allowed by the patient's insurance company, then code group 99241-99245 should be used for the consult request. Depending on whether a transfer of care is made or not, subsequent visits should be coded using either this same consult code group or the office established patient code group (99211-99215).
A 78 year old Medicare patient is referred by the primary care physician to a cardiology group for chest pain. A stress test, ordered the day prior, was read as abnormal by a different cardiologist in the same group practice.What should the cardiologist code for their initial E/M encounter? Based on the Medicare definition detailed above, reading of a stress test does not constitute professional services. It should be ignored when determining whether the patient is new or established. In addition, Medicare does not recognize consult codes. Cardiology is a Medicare recognized specialty. If the patient has received any professional services (E/M service or other face-to-face service) by any cardiologist or NPP working under the direction of the cardiologist or any other cardiologist in the same group practice in the last three years, only the established patient clinic code group 99211-99215 can be used. If no cardiologist or NPP working with a cardiologist in this group practice has seen the patient in the last three years, then the patient is a new patient. Code group 99201-99205 should be used for the initial visit.
NURSE PRACTITIONER AND PHYSICIAN ASSISTANT E/M VISIT SCENARIO
Qualified non-physician practitioners are considered part of the group practice and specialty for which they provide service along with physicians in the same specialty and group practice. In fact, Medicare's E/M Services Guide (on page 7 linked above) states quite clearly that non-physician practitioners are treated the same as physicians as providers of professional services over the three year time frame. Even the CPT® definition bundles the physician with qualified health care professional in their definition of new vs. established patients. In addition, the 2014 CPT® manual says
When advanced practice nurses and physician assistants are working with physicians they are considered as working in the exact same specialty and exact same subspecialties as the physician.
ON CALL AND CROSS-COVERING PROFESSIONAL SERVICES SCENARIO
If a physician or other qualified NPP is providing cross-cover care for another physician, how does this affect the new or established patient decision? The answer to this question has been answered by WPS, a Medicare contractor.
In the instance where a physician is on call for or covering for another physician, the patient's encounter will be classified as it would have been by the physician who is not available.The 2014 CPT® manual says
In the instance where a physician/qualified health care professional is on call for or covering for another physician/qualified health care professional, the patient's encounter will be classified as it would have been by the physician/qualified health care professional who is not available.I find this guidance interesting and conflicting with the definition of a new patient. If one solo practitioner is providing coverage for another solo practitioner in a different group practice, they have different tax identification numbers. By their own admission, Medicare states they audit the new vs. established patient decision based on the tax identification number. Their computer algorithms may not be able to establish an on call or cross-covering scenario in situations where two physicians, whether of like specialty or not, of different groups with different tax identification numbers, are providing coverage for each other.
When would this scenario occur? Consider the hospital observation scenario where one physician is providing on call services for another physician and they are asked to consult on a Medicare observation patient being admitted to the hospital by another group practice. It may be possible the on call physician has not seen the patient in the last three years but the patient's normal physician has. Should the cross-covering physician bill for a new patient encounter or an established patient encounter? According to CMS and CPT® guidance, the on call physician should bill as if they were the patient's normal physician. However, if they choose to bill the E/M visit as a new patient encounter, it may be difficult for computer algorithms to identify this coding error due to the different tax identification numbers used by both physicians. In fact, the covering physician wouldn't even know whether the patient had professional services provided by the patient's normal physician in the prior three years as they probably would not have access to their office records.
MULTIPLE PRACTICE SITES, SAME TAX ID SCENARIO
Consider the scenario where a family practice group has multiple sites of care all billing under the same tax identification number. Each site has their own patient records that are not available at other clinic sites. The patient is now being evaluated at a clinic site by a different physician or NPP who has never seen the patient and has no records available. Should this patient be coded as a new patient or an established patient? If a patient has been seen in the previous three years by any physician or NPP in the same group and specialty, regardless of which clinic site they went to and regardless of whether patient records are available, only established patient codes should be used. CMS and CPT® rules do not provide exceptions to practice sites that do not have access to records.
Site of service also does not apply if the patient received professional services in the hospital or in the emergency department. Consider the scenario where Physician A provides inpatient hospital care for a patient. The patient has never been seen previously by Physician A or any other physician or NPP in the same specialty and same group practice of Physician A. The patient is discharged and fails to follow up as requested. Two years later the patient calls the office of Physician A requesting to establish care in the clinic with Physician A. Because Physician A has provided professional services in the last three years, the patient is considered an established patient, regardless of which physician or NPP in the in the same specialty and group practice provides the care.
CHANGE IN GROUP PRACTICE SCENARIO
How should a physician or NPP code patients after they have left one group practice and joined another? Under a new group or solo practice, the physician would have a new tax identification number. However, the definition of a new patient says they cannot have received professional services in the last three years from the physician or qualified health care professional. Some payer algorithms may not be able to identify the new vs. established patient decision for physicians or NPP who change tax identifications. Some may. To bill and code correctly the correct interpretation of this scenario says to bill established patient care codes if the physician or NPP has seen the patient for professional services in the last three years.
What if a physician changes groups and one of their established patients is seen in the new group for the first time by a physician or non-physician practitioner in the new group who has never seen the patient and has no records on the patient? Since the patient is established to the physician new to the group, the patient is established to all physicians and qualified health care professionals in the group. Established care codes should be used.
RECOVERY AUDITORS AND NEW PATIENT CODES
Physicians and other non-physician practitioners should be aware that Recovery Auditors, under contract from CMS, are specifically targeting improper payments involving new patient claims when the beneficiary does not meet defined criteria to be a new patient. Medicare Learning Network document MM8165 says
As a result of overpayments for new patient E&M services that should have been paid as established patient E&M services, CMS will implement changes to the Common Working File (CWF) to prompt CMS contractors to validate that there are not two new patient CPTs being paid within a three year period of time.Which codes will be checked? This document further clarifies which codes the Recovery Auditors will be checking.
The new patient CPT codes that will be checked in these edits include 99201- 99205, 99324 - 99328, 99341 - 99345, 99381 - 99387, 92002, and 92004. The edits will also check to ensure that a claim with one of these new patient CPT codes is not paid subsequent to payment of a claim with an established patient CPT code (99211 - 99215, 99334 - 99337, 99347 - 99350, 99391 - 99397, 92012, and 92014) .Given the desire of CMS to recuperate overpayments and the complexity of the rules to follow, I encourage all physicians to be diligent in determining when their patient is a new patient or an established patient by CMS criteria.
RVU OF NEW AND ESTABLISHED CLINIC PATIENTS
What is the difference in relative value unit (RVU) for the new and established common outpatient clinic codes? In 2016, the work RVU (wRVU) values of these common codes are described here. I have provided a more detailed RVU and dollar analysis at each linked CPT® lecture below. As you can see, the difference in work RVU value (and total RVU value) is quite significant for similar levels of service when comparing new vs. established care codes.
LINK TO E/M POCKET REFERENCE CARD POST
|

Tweet