It’s been about six years since the passage of the Affordable Care Act, but some provisions of the health care law that can improve health care options for small businesses are still being implemented – like employee choice. By learning about this addition and other aspects of the law, small business owners can empower themselves to make the best decisions regarding health coverage for themselves and their employees. In many ways, health care options for small businesses are remaining the same this year. For instance, the Small Business Health Options Program in Illinois will continue offering an array of cost-competitive insurance plans from which employers can choose. And as always, qualified small businesses that purchase health insurance through SHOP may receive federal tax credits to help offset the cost of coverage.
It’s been about six years since the passage of the Affordable Care Act, but some provisions of the health care law that can improve health care options for small businesses are still being implemented – like employee choice. By learning about this addition and other aspects of the law, small business owners can empower themselves to make the best decisions regarding health coverage for themselves and their employees. In many ways, health care options for small businesses are remaining the same this year. For instance, the Small Business Health Options Program in Illinois will continue offering an array of cost-competitive insurance plans from which employers can choose. And as always, qualified small businesses that purchase health insurance through SHOP may receive federal tax credits to help offset the cost of coverage.
Employee Choice, a Positive New Change
There are several new features of the law being implemented this year, though. One of the biggest and most promising changes is the implementation of employee choice, which is now available in every state. Employee choice allows small business workers to choose from a number of plans from different insurance carriers. Under employee choice, workers choose which carrier they’d prefer to use, instead of business owners choosing for them. This option plays a key role in distinguishing SHOP from the outside health insurance market, and it’s popular among small business owners. In fact, Small Business Majority’s polling found two-thirds of small employers believe allowing employees to choose among multiple carriers is an important element of the health care marketplaces.
While employee choice is a great development for small businesses, options under Illinois’s employee choice program aren’t as robust as they could be. In some parts of Illinois, only one or two insurance providers are participating in SHOP. While employers can still choose different levels of coverage from participating providers, more providers will need to participate to boost options for small businesses.
Taking Advantage of the New Opportunities
If your business has fewer than 51 full-time employees, you can enroll in SHOP at any time during the year to take advantage of employee choice. In order to begin the enrollment process now, entrepreneurs should visit www.getcoveredillinois.gov or the National Association of Health Underwriters to contact a health insurance broker who is trained and certified to enroll small businesses for SHOP Marketplace plans. Brokers are well-versed in the ins-and-outs of the ACA, and there’s often no extra cost to utilize their services.
While 2016 offers changes in Illinois’s small business health insurance landscape, small business owners shouldn’t be concerned. Changes like employee choice are a step in the right direction for entrepreneurs. The best bet is for employers to arm themselves with information; that way, they can choose health coverage that maximizes benefits for their business.
Geri Aglipay
Outreach Manager, Midwest Region and Greater Chicago
Small Business Majority
99306 CPT® Code Description, Progress Notes, RVU, Distribution (Level 3 Initial Nursing Facility Care)
This 99306 CPT® lecture reviews the procedure code definition, progress note examples, RVU values, national distribution data and explains when this code should be used in the nursing facility setting (nursing home). CPT stands for Current Procedural Terminology. This code is part of a family of medical billing codes described by the numbers 99304-99306. CPT® 99306 represents the high (level 3) initial nursing facility care visit (whether you are the attending or a consultant) and is part of the Healthcare Common Procedure Coding System (HCPCS). This procedure code lecture for initial nursing facility care, to be used for new or established patients, is part of a complete series of CPT® lectures written by myself, a board certified internal medicine physician with over ten years of clinical hospitalist experience in a large community hospitalist program. I have written my collection of evaluation and management (E/M) lectures over the years to help physicians and nonphysician practitioners (nurse practitioners, clinical nurse specialists, certified nurse midwives and physician assistants) understand the complex criteria needed to stay compliant with the Centers for Medicare & Medicaid Services (CMS) and other third party insurance companies.
You can find my entire collection of medical billing and coding CPT® lectures together in one place on my Pinterest site (CPT® lectures here and other associated E/M lectures here). You don't need to be a Pinterest member to get access to any of my CPT® procedure lectures. As you gain understanding of these E/M procedure codes, remember you have an obligation to make sure your documentation supports the level of service you are submitting for payment. The volume of your documentation should not be used to determine your level of service. The details of your documentation are what matter most. In addition, the E/M services guide says the care you provide must be "reasonable and necessary" and all entries should be dated and contain a CMS defined legible signature or signature attestation, if necessary.
My interpretations discussed below are based on my review of the 1995 and 1997 E&M guidelines, the CMS E&M guide and the Marshfield Clinic audit point system for medical decision making. These resources can be found in my hospitalist resources section. The Marshfield Clinic point system is voluntary for Medicare carriers but has become the standard audit compliance tool in many parts of the country. You should check with your own Medicare carrier in your state to verify whether or not they use a different criteria standard than that for which I have presented here in my free educational discussion. I recommend all readers obtain their own updated CPT® reference book as the definitive authority on CPT® coding. I have provided access through Amazon to the 2016 CPT® standard edition pictured below and to the right. CPT® 99306 is a new or established patient procedure code and can be used by certain qualified healthcare practitioners to get paid for their initial admission or consulting role for initial nursing facility care. The American Medical Association (AMA) describes the 99306 CPT® procedure code as follows:

 Initial nursing facility care, per day, for the evaluation and management of a patient, which requires these 3 key components: A comprehensive history; A comprehensive examination; Medical decision making of high complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient's and/or family's needs. Usually, the presenting problem(s) are of high severity. Typically, 45 minutes are spent at the bedside and on the patient's facility floor or unit.
Initial nursing facility care, per day, for the evaluation and management of a patient, which requires these 3 key components: A comprehensive history; A comprehensive examination; Medical decision making of high complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient's and/or family's needs. Usually, the presenting problem(s) are of high severity. Typically, 45 minutes are spent at the bedside and on the patient's facility floor or unit.
The initial nursing facility care codes should be used whether the patient is an established patient or a new patient to the provider. An established patient is defined as an individual who has received professional services from a doctor or other qualified health professional of the exact same specialty and subspecialty who belonged to the same group practice within the past three years.
This medical billing code can be used for time based billing when certain requirements are met. However, documentation of time is not required to remain compliant with CMS regulations. If billed without time as a consideration, CPT® 99306 documentation should comply with the rules established by the 1995 or 1997 guidelines referenced above. The three important coding components for an inintial nursing facility care note are the:
Documentation requirements for a CPT®99306 initial nursing facility encounter are as follows:
This patient meets criteria for a level three initial nursing care facility care code because it contains all the required medically necessary and reasonable elements for a comprehensive history, a comprehensive physical exam and high complexity medical decision making. Note, the only documentation difference between a level 3 (CPT ® 99306) initial nursing facility care evaluation and the level 2 (CPT® 99305) initial nursing facility care evaluation is the requirement for high vs moderate complexity in MDM respectively. History and physical exam element requirements are otherwise identical.
Medical decision making in this initial encounter is high complexity because this patient achieved 4 points for a new problem with further workup planned under the diagnosis component and they received 4 points under the data portion as well (1 + 1 + 2). In this clinical example, the risk table does not apply. However, I use the risk table every day to qualify my patients for level three initial care codes. I think physicians constantly underestimate their level of risk because they deal with the same medical problems day in and day out and their daily encounters do not appear risky to them. But remember, the risk is for the patient, not for the physician. Documentation of high risk drug toxicity is frequently underestimated when choosing the level of E/M service. I highly recommend physicians read and understand the risk table to better understand why they are likely undercoding every day.
The point system detailed above is part of the Marshfield Clinic audit tool I use every day with my bedside E/M pocket cards detailed below. High impact risk table elements are part of these cards. I use them to make sure my billing and coding accurately reflects the level of service I provide. Why am I able to document the things I did above and have it comply with E/M rules? Detailed next are important points to remember when documenting the history, physical exam and MDM. This information is referenced in detail directly from the E/M services guide linked above.
The information detailed below comes straight from the E/M services guide. Read and understand these important nuggets of information. What and how you document is far more important than the volume you document. Providing auditors with documentation you have provided the services listed below will elevate your level of service quite rapidly into higher levels of E/M service. You are already providing this service. Let CMS give you credit for the work you are doing, but are probably forgetting to document appropriately. Remember to document, document, document.
The Centers for Medicare & Medicaid Services (CMS) has rules defining which qualified healthcare professionals are allowed to bill for the initial nursing facility (NF) care encounter. Medical Learning Network Matters documents MM4246 and SE1308 and this summary document are great resources to help providers navigate these complex rules. Briefly, Medicare distinguishes between delegation of physician visits in skilled nursing facilities (SNF -- Place of Service Code 31, for patients in a Part A SNF stay), and nursing facilities (NF -- Place of Service Code 32, for patients who do not have Part A SNF benefits, patients who are in a nursing facility or in a non-covered SNF stay). The setting is determined by whether the visit to a patient in a certified bed is to a resident whose care is paid for by Medicare Part A in a SNF or to a resident whose care is paid for by Medicaid in a NF.
Prolonged service codes (CPT® 99356 and 99357) are allowed for medically necessary prolonged care services for code groups 99304-99306 (initial nursing facility care) and 99307-99310 (subsequent nursing facility care) and 99318 (annual nursing facility assessment).
Per the Medicare Claims Manual 30.6.9.2.D (page 60)
No. Per the August 2015 CMS Manual Change Request 9231 (page 13):
Medicare Contractor WPS provided this insight during their question and answer publication here:
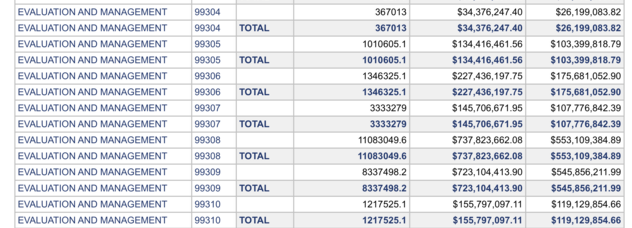
What is the distribution of CPT® code 99306 relative to other levels of service in this medical code group (99304-99306)? Data from the most recent 2014 CMS Part B National Procedure Summary Files data (2014 zip file) shows how many CPT® 99306 encounters were billed and the dollar value of their services for Part B Medicare. As you can see in the image below, E/M code 99306 had 1,346,325 allowed services in 2014 with allowed charges of $227,436,197.75 and payments of $175,681,052.90. Based on a review of the summary file, a total of 2,723943 visits were allowed for 99304-99306 in 2014. The code CPT®99306 was used 49.4% of the time in this code group (99304-99306).
Tweet
You can find my entire collection of medical billing and coding CPT® lectures together in one place on my Pinterest site (CPT® lectures here and other associated E/M lectures here). You don't need to be a Pinterest member to get access to any of my CPT® procedure lectures. As you gain understanding of these E/M procedure codes, remember you have an obligation to make sure your documentation supports the level of service you are submitting for payment. The volume of your documentation should not be used to determine your level of service. The details of your documentation are what matter most. In addition, the E/M services guide says the care you provide must be "reasonable and necessary" and all entries should be dated and contain a CMS defined legible signature or signature attestation, if necessary.
99306 MEDICAL CODE DESCRIPTION
My interpretations discussed below are based on my review of the 1995 and 1997 E&M guidelines, the CMS E&M guide and the Marshfield Clinic audit point system for medical decision making. These resources can be found in my hospitalist resources section. The Marshfield Clinic point system is voluntary for Medicare carriers but has become the standard audit compliance tool in many parts of the country. You should check with your own Medicare carrier in your state to verify whether or not they use a different criteria standard than that for which I have presented here in my free educational discussion. I recommend all readers obtain their own updated CPT® reference book as the definitive authority on CPT® coding. I have provided access through Amazon to the 2016 CPT® standard edition pictured below and to the right. CPT® 99306 is a new or established patient procedure code and can be used by certain qualified healthcare practitioners to get paid for their initial admission or consulting role for initial nursing facility care. The American Medical Association (AMA) describes the 99306 CPT® procedure code as follows:

The initial nursing facility care codes should be used whether the patient is an established patient or a new patient to the provider. An established patient is defined as an individual who has received professional services from a doctor or other qualified health professional of the exact same specialty and subspecialty who belonged to the same group practice within the past three years.
This medical billing code can be used for time based billing when certain requirements are met. However, documentation of time is not required to remain compliant with CMS regulations. If billed without time as a consideration, CPT® 99306 documentation should comply with the rules established by the 1995 or 1997 guidelines referenced above. The three important coding components for an inintial nursing facility care note are the:
- History
- Physical Exam
- Medical Decision Making Complexity
“Incident to” E/M visits, provided in a facility setting, are not payable under the Physician Fee Schedule for Medicare Part B. Where a physician establishes an office in a facility, the “Incident to” E/M visits and requirements are confined to this discrete part of a SNF/NF designated as his/her office. The place of service (POS) on the claim should be “office” (POS 11).
Documentation requirements for a CPT®99306 initial nursing facility encounter are as follows:
- Comprehensive history: Requires 4 or more elements of the history of present illness (HPI) OR documentation of the status of THREE chronic medical conditions. At least one item each from past history (illnesses, operations, injuries, treatments), social history and family history is also required. In addition, a complete review of systems is also required (10 or more organ systems).
- Comprehensive examination: The CMS E&M services guide on pages 29 and 30 describe the acceptable body areas and organ systems for physical exam. Either a general multi-system examination or complete examination of a single organ system (with other symptomatic or related body area(s) or organ system(s)--1997 guidelines) is acceptable. For a general multi-system examination, 1997 guidelines require documentation of at least two bullets each in at least nine organs systems or body areas (described on pages 50-53 in E/M services guide) while 1995 guidelines require findings from about 8 or more of the 12 organ systems, not otherwise specified. Requirements for a complete single organ exam are discussed in the E/M services guide from pages 57-79.
- Medical decision making of high complexity (MDM): This is split into three components. The 2 out of 3 highest levels in MDM are used to determine the overall level of MDM. The level is determined by a complex system of points and risk. What are the three components of MDM and what are the the minimum required number of points and risk level as defined by the Marshfield Clinic audit tool?
- Diagnosis (4 points)
- Data (4 points)
- Risk (high); The risk table can be found on page 35.
CLINICAL EXAMPLE OF CPT® 99306
Here is a note for a high level initial nursing facility encounter (CPT® 99306) for new or established patients. In this case, an internist is being asked to evaluate a patient as a consultant at the request of the nursing facility physician attending.
C/C: My leg is redHPI: 78yo female with calf pain. Admitted for weakness to the SNF following a recent stroke. She has left lower extremity 6/10, dull and constant pain that started two days ago and is associated with edema and erythema. Internist was asked to evaluated as a consultant at the request of the rehab physician. (4 elements from HPI)PFSH: Recent stroke, HTN, HLP. on Lipitor, aspirin, and lisinopril. Quit smoking on the day of her hospital admission 6 days ago. Mother with a history of stroke. (All 3 elements documented)ROS: Except as dictated above, all other systems were reviewed and otherwise negative without further pertinent positives or negatives (10+ROS documented. This notation is allowable under E/M rules)Exam: 120/80 85 102.7 temp, well appearing (9 organ systems with at least 2 bullets each)Neurological: Mild residual weakness in left leg and arm following stroke. Cranial nerves intact.HENT: NormalEyes: NormalCV: NormalRespiratory: NormalGI: NormalPsychiatric: NormalLymphatic: NormalSkin: Edema, warmth, redness left leg, lines consistent with cellulitis, marked with skin marker.
LabsWBC 13K (1 point for documenting lab in complexity of data decision making section). Venous Doppler report reviewed. No clot. (1 point for documenting review of a vascular study report in complexity of data decision making).Impression
- Cellulitis (4 points for new problem, further workup planned under the number of diagnosis for medical decision making)
PlanStart antibiotics. Reviewed case details with rehab physician Vitals stable except for fever. Initiate oral antibiotics. Check a sed rate and xray of the leg to verify no fracture from falling after stroke. Reviewed old records, no xray done during acute care stay in the hospital (2 points for documenting discussion of case with another health care provider/reviewing old records). Continue work up with followup lab in am. Follow glucose to verify lack of diabetes as this can change antibiotic coverage decisions. Follow Cr to adjust antibiotic dosing. See orders for full details.
Medical decision making in this initial encounter is high complexity because this patient achieved 4 points for a new problem with further workup planned under the diagnosis component and they received 4 points under the data portion as well (1 + 1 + 2). In this clinical example, the risk table does not apply. However, I use the risk table every day to qualify my patients for level three initial care codes. I think physicians constantly underestimate their level of risk because they deal with the same medical problems day in and day out and their daily encounters do not appear risky to them. But remember, the risk is for the patient, not for the physician. Documentation of high risk drug toxicity is frequently underestimated when choosing the level of E/M service. I highly recommend physicians read and understand the risk table to better understand why they are likely undercoding every day.
The point system detailed above is part of the Marshfield Clinic audit tool I use every day with my bedside E/M pocket cards detailed below. High impact risk table elements are part of these cards. I use them to make sure my billing and coding accurately reflects the level of service I provide. Why am I able to document the things I did above and have it comply with E/M rules? Detailed next are important points to remember when documenting the history, physical exam and MDM. This information is referenced in detail directly from the E/M services guide linked above.
E/M DOCUMENTATION PEARLS
- History
- The chief complaint, ROS and PFSH may be listed as separate elements or included in the description of the HPI.
- A ROS and PFSH obtained during an earlier encounter does not need to be re-recorded if there is evidence the physician reviewed and updated the previous information. This update may be documented by describing new ROS or PFSH information or noting there has been no change in the information and noting the date and location of the earlier ROS and or PMFSH. The E/M services guide does not place a time limit on how far back the previous documentation can be reviewed.
- The ROS and PFSH can be recorded by ancillary staff or on a form completed by the patient and the physician must note they have reviewed and confirmed the information and supplement any other relevant information.
- If the physician is unable to obtain a history from the patient or other source, the physician should describe the patient's condition which prevents obtaining a history.
- Physical Exam
- Specific abnormal and relevant negative findings of the affected or symptomatic body area(s) or organ systems(s) should be documented. Writing "abnormal" is not sufficient.
- Abnormal findings on exam should be described
- Writing "negative" or "normal" is sufficient to document normal findings related to unaffected areas or asymptomatic organ systems.
- Medical Decision Making (accurate documentation of these issue can quickly increase level of MDM service being provided):
- Number of Diagnoses and/or Management Options:
- Each diagnosis should have documentation that the problem is improved, controlled, resolving, resolved, uncontrolled, worsening or failing to change as expected.
- For problems without a diagnosis, the assessment may be stated in the form of a differential diagnosis such as possible, probable, or rule out diagnosis.
- Document the initiation or change in treatment.
- Amount and/or Complexity of Data to be Reviewed:
- Document a decision to obtain and review old medical records or obtain history from sources other than the patient, such as family or other caretakers.
- Document relevant findings from the review of old record or discussion with family or other caretakers. Simply documenting "Old records reviewed" or "additional history obtained from family" without elaboration is not enough.
- Document your discussion of contradictory or unexpected test results with the interpreting physician.
- Document you personally reviewed an image or tracing or specimen.
- Notations such as "wbc elevated" or "chest x-ray unremarkable" is acceptable.
- Risk or Significant Complications, Morbidity, and/or Mortality
- Remember to document comorbidities and other factors that increase the complexity of MDM by increasing the risk of complications, morbidity and mortality.
- Referral for urgent invasive procedures and surgeries should be documented or implied.
- USE THE TABLE OF RISK! That's what it's there for. I have detailed the most common risk elements I use in my daily practice on my E/M card shown below.
- There are many other points to consider when documenting MDM. There are too many to list here individually, but most are described in the MDM portion of my E/M bedside pocket cards detailed below. In addition, I recommend thoroughly reviewing pages 13 through 18 of the E/M services guide for a thorough understanding of the finer points of E/M coding.
MEDICARE RULES FOR INITIAL ENCOUNTER: PHYSICIAN VS QUALIFIED NONPHYSICIAN PRACTITIONER EVALUATION
The Centers for Medicare & Medicaid Services (CMS) has rules defining which qualified healthcare professionals are allowed to bill for the initial nursing facility (NF) care encounter. Medical Learning Network Matters documents MM4246 and SE1308 and this summary document are great resources to help providers navigate these complex rules. Briefly, Medicare distinguishes between delegation of physician visits in skilled nursing facilities (SNF -- Place of Service Code 31, for patients in a Part A SNF stay), and nursing facilities (NF -- Place of Service Code 32, for patients who do not have Part A SNF benefits, patients who are in a nursing facility or in a non-covered SNF stay). The setting is determined by whether the visit to a patient in a certified bed is to a resident whose care is paid for by Medicare Part A in a SNF or to a resident whose care is paid for by Medicaid in a NF.
SNF FACILITY RULES (PLACE OF SERVICE CODE 31)
The initial comprehensive visit in a SNF must be provided by a physician and must occur no later than 30 days after a resident's admission into the SNF. The physician may not delegate the initial visit to another qualified health professional in a SNF stay. However, after the initial comprehensive visit in a SNF (99304-99306) the physician may delegate future subsequent care visits (99307-99310) to other qualified nonphysician practitioners (NPP), whether they are employed by the facility or not. With these follow-up visits, physician co-signature is not required. Note also, no visits at SNFs may be billed as split/shared services.
NURSING FACILITY RULES (PLACE OF SERVICE CODE 32)
At the option of the state, any required physician task in a NF (including tasks which the regulations specify must be performed personally by the physician, such as the initial comprehensive evaluation) may also be satisfied when performed by qualified non-physician practitioners who are not an employee of the facility but who are working in collaboration with the physician and must be completed no later than 30 days after admission. That means, in this place of service code 32, the initial nursing facility encounter (99304-99306) can be delegated to qualified non-physician practitioners such as nurse practitioners (NPs), physician assistants (PAs) and clinical nurse specialists (CNSs) who are not employees of the facility but work in collaboration with the physician. They may also perform other required physician visits and medically necessary follow-up visits (99307-99310). Visits by non-physician practitioners employed by the NF may not take the place of the physician required visits, but can perform medically necessary visits and write orders based on those visits. Note also, no visits at NFs may be billed as split/shared services.
DUALLY-CERTIFIED FACILITIES (SNF/NFs)
In situations where beds are dually certified under Medicare and Medicaid, the facility must determine how the resident stay is being paid.
Medicare eliminated consult codes in 2010. So what code should a physician or qualified NPP use when evaluating a patient as a consultant for the initial visit in a SNF or NF? Transmittal 2282 from the CMS manual helps explain.
WHAT CODE TO USE WHEN CONSULTING IN A NURSING FACILITY
Medicare eliminated consult codes in 2010. So what code should a physician or qualified NPP use when evaluating a patient as a consultant for the initial visit in a SNF or NF? Transmittal 2282 from the CMS manual helps explain.
"The general policy of billing the most appropriate visit code, following the elimination of payments for consultation codes, shall also apply to billing initial visits provided in skilled nursing facilities (SNFs) and nursing facilities (NFs) by physicians and nonphysician practitioners (NPPs) who are not providing the federally mandated initial visit. If a physician or NPP is furnishing that practitioner’s first E/M service for a Medicare beneficiary in a SNF or NF during the patient’s facility stay, even if that service is provided prior to the federally mandated visit, the practitioner may bill the most appropriate E/M code that reflects the services the practitioner furnished, whether that code be an initial nursing facility care code (CPT codes 99304-99306) or a subsequent nursing facility care code (CPT codes 99307-99310) when documentation and medical necessity do not meet the requirements for billing an initial nursing facility care code."
ARE PROLONGED SERVICE CODES ALLOWED?
Prolonged service codes (CPT® 99356 and 99357) are allowed for medically necessary prolonged care services for code groups 99304-99306 (initial nursing facility care) and 99307-99310 (subsequent nursing facility care) and 99318 (annual nursing facility assessment).
CAN I BILL FOR ACUTE CARE HOSPITAL DISCHARGE AND NURSING CARE FACILITY ADMISSION ON THE SAME DATE?
Per the Medicare Claims Manual 30.6.9.2.D (page 60)
D. Hospital Discharge Management (CPT Codes 99238 and 99239) and Nursing Facility Admission Code When Patient Is Discharged From Hospital and Admitted to Nursing Facility on Same Day
A/B MACs (B) pay the hospital discharge code (codes 99238 or 99239) in addition to a nursing facility admission code when they are billed by the same physician with the same date of service.
CAN I BILL OFFICE OR ER VISIT AND INITIAL NURSING FACILITY CARE ON THE SAME DATE?
No. Per the August 2015 CMS Manual Change Request 9231 (page 13):
C. Office/Outpatient or Emergency Department E/M Visit on Day of Admission to Nursing FacilityMACs may not pay a physician for an emergency department visit or an office visit and a comprehensive nursing facility assessment on the same day. Bundle E/M visits on the same date provided in sites other than the nursing facility into the initial nursing facility care code when performed on the same date as the nursing facility admission by the same physician.
CAN I BILL FOR INITIAL NURSING FACILITY CARE IF I EVALUATE THEM AT A HOSPITAL BEFORE TRANSFER?
Medicare Contractor WPS provided this insight during their question and answer publication here:
Question 3: Can the admission to a Skilled Nursing Facility (SNF) or Nursing Facility (NF) be performed from the hospital? Is there a requirement that the patient must be seen physically in the home within a certain time period?
Answer: We received confirmation from CMS on this question. When the physician is performing the assessment for the admission to the SNF or NF at the hospital, the physician may bill this using place of service (POS) 31 - SNF or 32 - NF. If the patient is discharged from the hospital and admitted to the SNF or NF on the same day, both services may be approved by Medicare when the physician provides both services. You can find more information in the IOM Publication 100-04, Chapter 12, Section 30.6.9.2 D. There are requirements as to the time-frame for the assessment and plan of care for the patient in a SNF. You can find more information in the IOM Publication 100-04, Chapter 12, Section 30.6.13.
CAN I BILL A DISCHARGE AND ADMISSION ON THE SAME DATE TO AN INPATIENT REHABILITATION FACILITY (POINT OF SERVICE 61)
Medicare Contractor WPS provides more insight from here:Question 12: The patient is discharged from the acute care hospital and admitted to an Inpatient Rehabilitation Facility (IRF) on the same day. Can we bill a discharge visit and an admission on the same day when performed by the same physician?
Answer: No. The CMS IOM Publication 100-04, Chapter 12, Section 30.6.9.1.E states that when a transfer from one facility to another occurs, the physician may bill a subsequent hospital visit code.
DISTRIBUTION OF ESTABLISHED PATIENT CARE CODES
What is the distribution of CPT® code 99306 relative to other levels of service in this medical code group (99304-99306)? Data from the most recent 2014 CMS Part B National Procedure Summary Files data (2014 zip file) shows how many CPT® 99306 encounters were billed and the dollar value of their services for Part B Medicare. As you can see in the image below, E/M code 99306 had 1,346,325 allowed services in 2014 with allowed charges of $227,436,197.75 and payments of $175,681,052.90. Based on a review of the summary file, a total of 2,723943 visits were allowed for 99304-99306 in 2014. The code CPT®99306 was used 49.4% of the time in this code group (99304-99306).
RVU VALUE
How much money does a CPT® 99306 pay? That depends on what part of the country you live in and what insurance company you are billing. E/M procedure codes, like all CPT® billing codes, are paid in relative value units (RVUs). This complex RVU discussion has been had elsewhere on The Happy Hospitalist. For raw RVU values, for 2016 a CPT® 99306 is worth 4.68 total RVUs. The work RVU for 99306 is valued at 3.06. A complete list of RVU values on common hospitalist E/M codes is provided at the linked URL. What is the Medicare reimbursement for CPT® code 99306? In my state, a CPT® 99306 pays just over $158 in 2016. The dollar conversion factor for one RVU in 2016 is $35.8043.
My coding card taught me that I should be billing for the work I'm providing and it has taught me how to document appropriately. You can see many more of my E/M lectures by clicking through to the link provided here. If you need bedside help determining what level of care you have provided, I recommend reviewing the pocket card described below.
My coding card taught me that I should be billing for the work I'm providing and it has taught me how to document appropriately. You can see many more of my E/M lectures by clicking through to the link provided here. If you need bedside help determining what level of care you have provided, I recommend reviewing the pocket card described below.
LINK TO E/M POCKET CARD POST
|
Tweet