This lecture will assist physicians and other non-physician practitioners (NPPs) determine if their initial hospital admission note documentation meets criteria for a level 2 (mid level H&P) or a level 3 (high level H&P)
evaluation and management (E/M) code. Recovery Audit Contractors will likely continue to target high level initial hospital encounters for improper payments. Physicians and other NPPs must continue to pursue documentation education to prevent accusations of over billing and to prevent under billing for work provided. I am an internal medicine physician with over 10 years experience as a clinical hospitalist. Based on my decade of experience and exhaustive review of E/M coding criteria, I believe most level 2 H&P hospital admissions would qualify for a level 3 H&P if practitioners understood how to document work already being provided. The link above provides free access to dozens of billing and coding lectures I have written to help others quickly decipher the complex rules used to determine the correct CPT® code for most inpatient and outpatient hospital and clinic encounters.
CPT® DEFINITIONS
The American Medical Association's 2015 Standard Edition CPT® provides definitions of all E/M services. This valuable resource is available through Amazon by clicking on the image to the right and below. I have previously discussed level two initial inpatient and observation hospital admission (
CPT® 99222 and 99219) and level three initial inpatient and observation hospital admission (
CPT® 99223 and 99220) codes in detail and I recommend all readers thoroughly review these lectures at their convenience.


To simplify understanding of the differences between a level 2 and a level 3 hospital H&P, I will treat the criteria for a level two initial inpatient hospital admission (CPT® 99222) the same as a level two initial observation hospital admission (CPT® 99219) and I will treat the criteria for a level three initial inpatient hospital admission (CPT® 99223) the same as a level three initial observation hospital admission (CPT® 99220). In both cases, their criteria are equivalent for all intents and purposes.
LEVEL 2 CRITERIA
A level 2 initial hospital admission note requires documentation of a comprehensive history, a comprehensive examination and medical decision making of moderate complexity. Presenting problem(s) are usually of moderate severity (50 minutes).
LEVEL 3 CRITERIA
A level 3 initial hospital admission note requires documentation of a comprehensive history, a comprehensive examination and medical decision making of high complexity. Presenting problems are usually of high severity (70 minutes).
Supporting documentation required for a level two note is identical to a level three note for history and examination. Shown in red, the only difference is the complexity of the medical decision making that documentation supports. If an initial hospital admission note does not have documentation to support a comprehensive history and examination, the highest level of service that can be billed is a level 1 H&P (
99221 or 99218).
TIME The CPT® definitions also provide guidance on expected time for the encounter. However, time can only be used in conjunction with the rules of counseling and coordination of care.
Time based billing has been discussed elsewhere on The Happy Hospitalist and is not relevant to this discussion.
NATURE OF THE PRESENTING PROBLEMThe CPT® definitions also provide guidance on the nature of the presenting problem. How does one audit a note for moderate severity or high severity? The CPT® handbook attempts to define moderate severity and high severity. Unfortunately, they chose to use the words moderate and high within their own definition. This makes standardized interpretation difficult.
Moderate severity: A problem where the risk of morbidity without treatment is moderate, there is moderate risk of mortality without treatment; uncertain prognosis OR increased probability of prolonged functional impairment.
High severity: A problem where the risk of morbidity without treatment is high to extreme; there is a moderate to high risk of mortality without treatment OR high probability of severe, prolonged functional impairment.
These vague CPT® definitions are difficult to interpret in clinical practice. How does one audit moderate or high risk based on this CPT® guidance? One cannot. That's why these elements of the CPT® definition are rarely
enforced in audit scenarios without using alternative tools (discussed below) to define the level of risk and complexity. What may be moderate or high to one patient, doctor or specialty may be moderate or high to another. One could argue all patients that need to be admitted to the hospital risk a high probability of morbidity or mortality without treatment. That's why they are in the hospital.
CLINICAL EXAMPLES
Appendix C of the CPT® manual provides pages and pages of clinical examples for a level 2 and level 3 hospital admission. These examples are a tragic example of failure to appreciate the complexities of patient care. These one and two sentence scenarios cannot tell the whole picture nor do they represent the reality and complexity of patient encounters in real life. I provide two Internal Medicine examples below from the CPT® handbook.
Level 2 H&P (99222)Initial hospital visit for a 61-year-old male with history of previous myocardial infarction, who now complains of chest pain.
CPT® provides this scenario as an appropriate level 2 admission. I disagree. Consider the scenario where an emergency department physician recommends admission to the hospital for evaluation and management of this patient with chest pain and a known prior history of myocardial infarction. If the patient declined admission and left the emergency department against medical advice, any reasonable discharging physician would have an informed consent discussion with the patient detailing the high risk of death or disability. By default, that would make this presenting problem of high severity and in direct conflict with the assumption that this presenting problem was of moderate severity. However, a cardiologist, after reviewing the data in the emergency department may have a different perspective and believe safe discharge from the emergency department is acceptable with low risk for complications. There in lies the dilemma. Defining moderate and high severity is open to great interpretation and cannot be reliably audited for payment purposes. Therefor, it should not be audited without more definitive criteria.
Regardless of the inability to audit vague terminology such as moderate or high, these CPT® clinical examples are not representative of real life patients. Most patients do not present with single diseases. Their complexity rises exponentially with other comorbid conditions. I do not place faith on these CPT® examples for providing appropriate coding guidance. This is why alternative methods have been developed to define moderate and high complexity and risk in audit situations. Here is a CPT® example of a level 3 inpatient hospital admission.
Level 3 H&P (99223)Initial hospital visit for a 70-year-old male with cutaneous T-cell lymphoma who has developed fever and lymphadenopathy.
I agree. However, I also believe the vast majority of all hospital admissions are complex enough to warrant the highest level of service. That's why they are in the hospital. In addition, based on risk defining criteria that has been developed, thorough documentation of work provided will often provide confirmation of high complexity medical decision making.
DIFFERENCE BETWEEN A LEVEL 2 AND LEVEL 3 H&P
The audit components of a level 2 and a level 3 inpatient or observation hospital admission are exactly the same with the exception of the medical decision making (MDM) component. While CPT® definitions include reference to the severity of the presenting problem, I've established above how determining the level of service based on that criteria is impossible. Official CPT® examples do not represent the realities of clinical medicine. So how is the correct level of service determined? Based on the CPT® definitions, audit decisions are decided with a detailed analysis of history, examination and medical decision making documentation.
As discussed above, the history documentation requirements and the examination documentation requirements are identical for a level 2 and level 3 initial hospital admission note. An auditor, who may have no medical training, cannot reliably categorize medical decision making, risk or severity of a presenting problem as moderate or high without checkbox criteria to assist in their efforts. Even Medicare's own
Evaluation and Management Services Guide provides only vague instructions on determining the level of complexity for MDM. Enter the Marshfield Audit Clinic Tool and point system (reviewed below) that was developed to provide additional guidance and support. The only audit tool difference between a level 2 and a level 3 initial hospital admission is the medical decision making component. For a level 2 hospital H&P, documentation should support medical decision making of moderate complexity. For a level 3 hospital H&P, documentation should support medical decision making of high complexity. This is where the Marshfield Clinic Audit Tool provides guidance.
MEDICAL DECISION MAKING (MDM)
MARSHFIELD CLINIC AUDIT TOOL
Where did the Marshfield Clinic point system E/M tool come from? It was developed in the early 1990s at a 600 physician multi-site, multi-specialty, mostly office-based practice in Wisconsin where Medicare's 1995 EM guidelines were beta tested. This medical decision making point system audit tool was developed by clinic staff and their local Medicare carrier. These scoring tools never made it into the official guidelines, but are accepted as a standard audit tool by most carriers today. I have created an
E/M pocket guide as a rapid bedside decision tool that incorporates their guidance into clinical decisions. Details of this bedside reference can be found at the link provided just above. These cards are available for purchase. All proceeds are donated to charity.
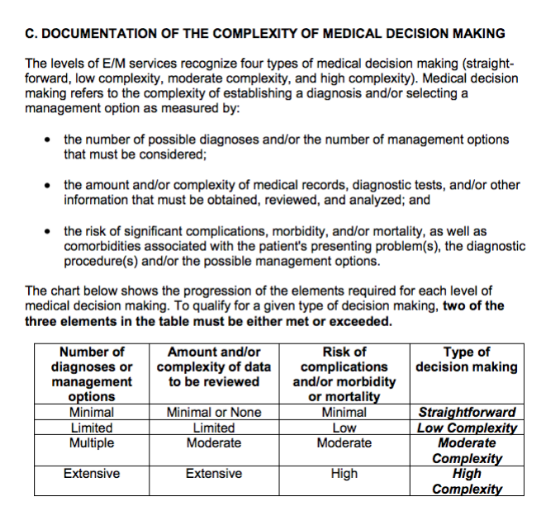
CMS GUIDANCE ON MEDICAL DECISION MAKING
Why do many Medicare carriers use the Marshfield Clinic Audit Tool to determine the correct level of service provided? Medicare's description of medical decision making in the
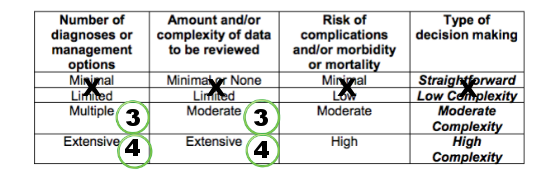
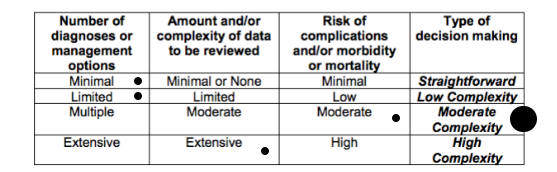
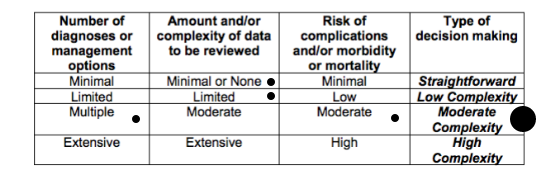
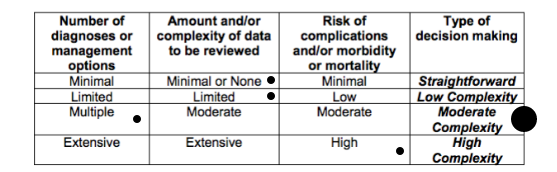
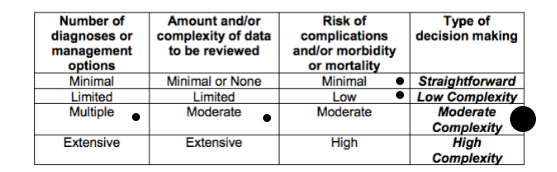
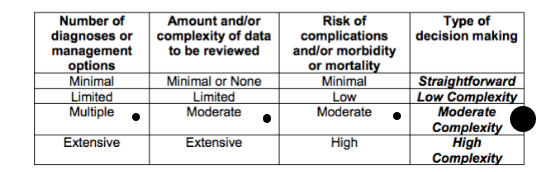
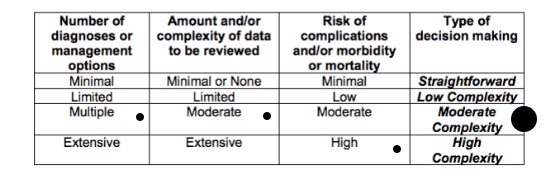
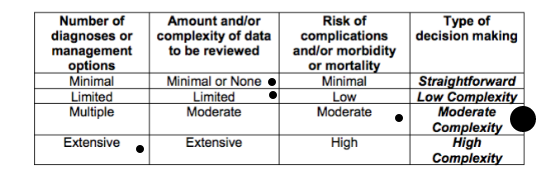
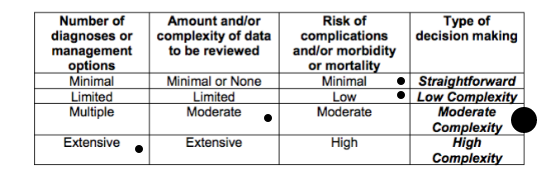
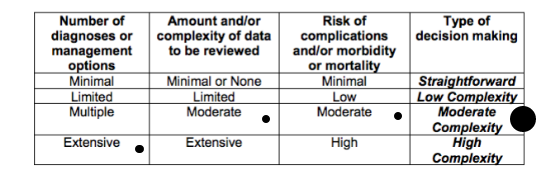
Evaluation and Management Services Guide (page 33) contains vague language that cannot be reliably reproduced in clinical practice. Here is a screen shot of the E/M Services Guide discussing medical decision making criteria.
How can a practitioner or auditor reliably determine when the number of diagnoses are multiple or extensive? How can a practitioner or auditor reliably determine when the amount and complexity of data is moderate or extensive? They can't. Ironically, determining the correct level of medical decision making complexity is complex. Just as the CPT® definitions use vague language in defining their codes, the E/M Services Guide also uses the same difficult language to
guide physicians and other NPPs. This is a tragedy. This is why The Marshfield Clinic Audit Tool for MDM was developed and used by auditors and practitioners to stay compliant. Pages
33-37 of the E/M Services Guide provides the basis for the Marshfield Clinic Audit Tool point system shown above on The Happy Hospitalist's bedside pocket E/M reference card. It provides quick access to documentation elements converted into Marshfield Clinic Audit Tool points. It may also help providers remember to document work provided but rarely described in the chart in order to get credit for documentation elements in an audit situation. For example, in the number of diagnoses or management options component of medical decision making, four points is given for a new problem with more workup planned when using the Marshfield Clinic Audit Tool. This is based on Medicare's E/M Services Guide (page 34) description of diagnosis complexity here.
The number and type of diagnostic tests employed may be an indicator of the number of possible diagnoses. Problems which are improving or resolving are less complex than those which are worsening or failing to change as expected.
This same point system applies to the amount and/or complexity of data to be reviewed. For example, one point is given for review or ordering of laboratory services in the Marshfield Clinic Audit Tool. This decision is based on Medicare's E/M Services Guide (page 35) description of amount and/or complexity of data to be reviewed.
If a diagnostic service (test or procedure) is ordered, planned, scheduled, or performed at the time of the E/M encounter, the type of service, eg, lab or x-ray, should be documented.
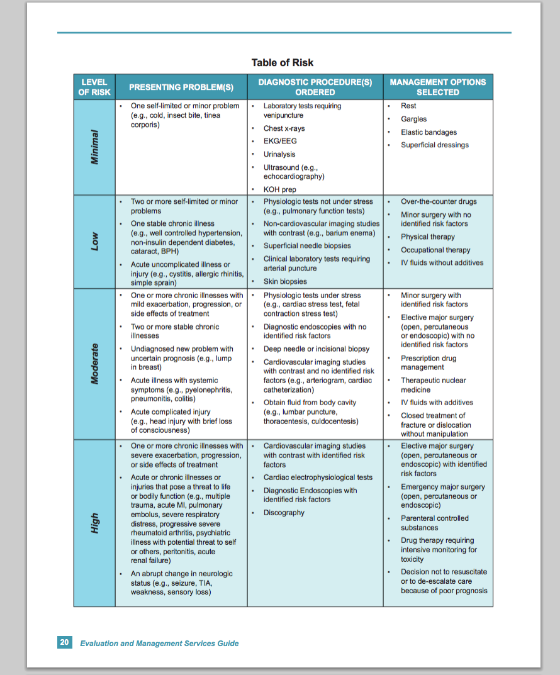
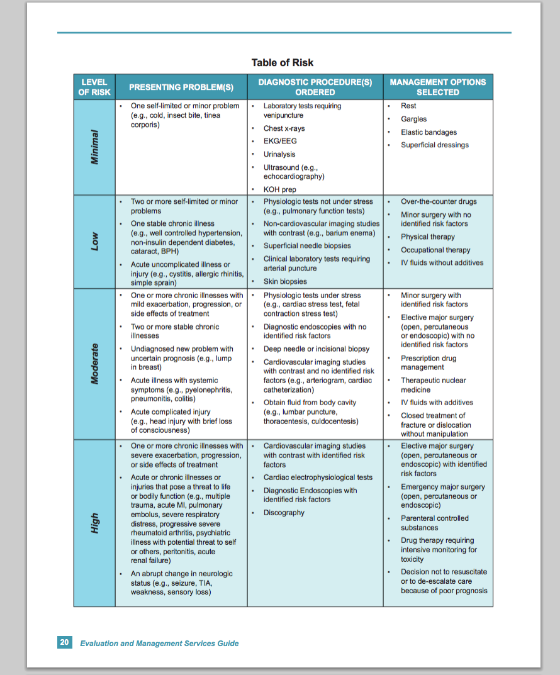
Medicare does provide decent guidance on risk of complications and/or morbidity or mortality with their risk table (shown below). However, some elements within this table contain vague language that can be open to interpretation and require physicians and other NPPs to document their thought processes aggressively to avoid accusations of incorrect billing when they believe high risk to the patient is present. Drug therapy requiring intensive monitoring is one such element. I have provided a detailed review of that component
here.
SIDE-BY-SIDE MDM CRITERIA COMPARISON
If you feel lost in this discussion, now is the time to place close attention. When combined with history and examination documentation, the MDM makes up the final necessary component for determining the correct CPT® code. Remember, the history and examination documentation required for a level 2 and level 3 hospital H&P admission are identical. Both require the highest level of service. For history, documentation must include at least four HPI elements or the status of three relevant chronic medical conditions, 10 or more review of systems and at least one element each from past history, family history and social history. For examination, documentation generally requires at least 2 bullets each from 9 organ systems, although I recommend readers review different examination documentation options available at the 99222 and 99223 links near the top of this lecture.
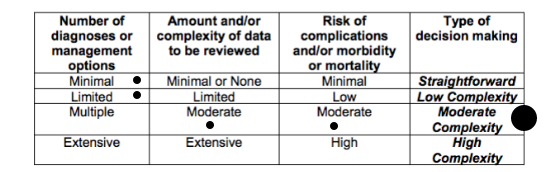
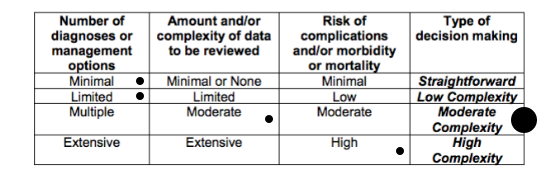
The only documentation difference between level 2 and a level 3 hospital H&P admission is in the medical decision making component. I will try my best to tie it all together and show you just how similar a level 2 and level 3 admit are in their medical decision making elements. Using Medicare's E/M Services Guide as a reference, I have incorporated the Marshfield Clinic point system as a side-by-side reference below.
Within the diagnosis and data elements of MDM, points are provided for defined elements of documentation found during a chart audit. For example, one point is allowed for a self limiting or minor problem in the diagnosis section of MDM while one point may be given for evidence the provider requested prior records. This is the basis of the point system under the Marshfield Clinic Audit Tool that is used by most Medicare carriers.
While this point system is not officially part of Medicare's E/M Services Guide, the risk table is. The risk table is available on
page 20 or 37 of the Evaluation and Management Services Guide. I have provided a screen shot here for quick reference. The highest element anywhere on the risk table determines the highest overall level of risk on the risk table. For example, a patient with an abrupt change in neurological status meets criteria for high risk on the risk table regardless of any other data points on the table.
To determine the overall level of MDM complexity, the highest two out of three elements from diagnoses, data and risk determine the overall level of MDM. In other words, the highest level of documentation for data and diagnosis, data and risk or diagnosis and risk will determine the overall level of MDM. Below are the minimum MDM criteria for a level 2 and level 3 initial hospital admission. For example a patient who's documentation supports 3 diagnosis points, 1 data point and moderate risk would qualify for level 2 MDM. A patient who's documentation supports 2 diagnosis points, 4 data points and high risk would qualify for level 3 MDM. A patient who's documentation supports 2 diagnosis points, 2 data points and high risk would not qualify for either level 2 or level 3 MDM for an initial hospital admission.
LEVEL 2 MDM (highest 2 out of 3 determines overall level of MDM)
DIAGNOSIS: 3 points
DATA: 3 points
RISK TABLE: moderate
LEVEL 3 MDM (highest 2 out of 3 determines overall level of MDM)
DIAGNOSIS: 4 points
DATA: 4 points
RISK TABLE: high
LEVEL 2 PERMUTATIONS
Here are all eleven potential documentation permutations for medical decision making of a level 2 hospital H&P admission. Remember, the two out three highest levels of documentation in diagnosis, data and risk will determine the overall level of MDM. This same exercise can be done to determine a level 3 hospital H&P admission as well.
Remember to always consider medical necessity. For example, ordering a stress test to increase the complexity of medical decision making on a chief complaint of big toe pain may raise some red flags if the chart undergoes an audit. I believe if you're anywhere in the ball park of practicing standard of care, justifying medical necessity will rarely be a determining factor in having to support your level of care based.
A level 2 hospital admit E/M service could often meet documentation audit criteria for a level 3 hospital admit if providers documented work already being provided but not described. Some coders may say high risk must be present to meet criteria for a level 3 admit. These coders are not following the rules provided by Medicare's Evaluation and Management Services Guide. In reference to diagnoses, data and risk, page 33 of the E/M Services Guide says:
To qualify for a given type of decision making, two of the three elements in the table must be either met or exceeded.
I again direct the provider and their coders to the E/M Services Guide as their reference point. The Marshfield Clinic Audit Tool was developed because of the vague language and difficulty in interpreting rules in Medicare's E/M Services Guide. High complexity medical decision making can be met based on diagnoses and data elements. As I have said before, make sure your workup is consistent with standard of care and medical necessity should never be an issue.
WHERE CAN I GET A COPY OF THE POINT SYSTEM?
Many examples of the Marshfield Clinic point system are available on the internet. Page two of this
Codeapedia reference provides a detailed description of the point system. This point system is the basis for the bedside E/M reference card provided by The Happy Hospitalist pictured above and
linked here again for easy reference.
MANY LEVEL 2s ARE PROBABLY LEVEL 3s
Practitioners who know how to accurately document their work are probably providing high complexity medical decision making in greater than 95% of their hospital admissions when they understand the elements of the risk table and are educated about the elements of the Marshfield Clinic Audit Tool point system. Remember, a level 2 hospital admission has the same history and and examination requirements as a level 3 hospital admission. All patients who are sick enough to be admitted or observed in a hospital setting should meet medical necessity for the highest level of history and examination. Medical necessity should never be questioned in these patients
In reality, many physicians and other NPPs are scared to bill too many level 3 admit notes for fear of getting audited. No fear should exist if documentation supports level 3 work already being provided. If all providers would document work they are already providing and billed appropriately, level 3 hospital admission distribution would rise dramatically and physician outliers, who are coding correctly, would disappear. Practitioners worried about getting audited as an outlier should continue to document work they are already providing and to bill correctly, regardless of their status as an outlier. Being an outlier is not fraudulent when documentation supports correct coding decisions. It's quite possible that most physicians who aren't billing mostly level 3 hospital admissions are the outliers because they either don't document work they are already providing, are not providing work that is medically necessary or are intentionally under billing for fear of an audit.
RVU COMPARISON
Most E/M services are given a relative value unit (RVU) value by CMS. I have previously
discussed RVUs. The most updated table of RVU values can be
found here. The difference in relative value units assigned to a level 2 vs. a level 3 H&P hospital admission are significant. For practitioners who's compensation may be determined by productivity, coding accurately for work already being provided can boost payments significantly. What are the RVU values for a level 2 and level 3 hospital admission? For Medicare patients in 2016,
one RVU is worth $35.8043.
LEVEL 2- Observation (99219) - work RVU 2.60; total RVU 3.80
- Inpatient (99222) - work RVU2.61; total RVU 3.87
LEVEL 3
- Observation (99220) - work RVU 3.56; total RVU 5.20
- Inpatient (99223) - work RVU 3.86; total RVU 5.70
A level 3 hospital H&P admission is valued 50% higher than a level 2 hospital H&P admission based on total RVU and nearly 48% higher based on work RVU. This difference is significant.
DISTRIBUTION OF LEVEL 2 vs. LEVEL 3 HOSPITAL ADMISSIONS
What is the distribution of level 2 and level 3 hospital admissions? This can vary depending on specialty. SHM/MGMA data from 2012 suggested CPT® codes 99222 and 99223 were utilized 29% and 66% of the time respectively with CPT® 99221 used just 2% of the time. Other Medicare distribution data is available at the CPT® 99222 and CPT® 99223 articles linked near the top of this lecture. These distribution numbers confirm similarity with SHM/MGMA data.
PAYMENT COMPARISON
Payments will vary based on geographical location. Providers in New York would generally get paid more than providers in Kansas. For example, in some localities, a level 2 hospital admission pays around $130 and a level 3 hospital admission pays around $190, a nearly 50% increase. Failure to document work already being provided can be expensive. Using distribution data, here are a few brief calculations assuming a hospitalist provides 600 Medicare admissions in a year. Using SHM/MGMA data (66% level 3 and 29% level 2), payment for these admissions would be (396 x $190) + (174 x $130) = $75, 240. This does not include the 5% utilization of 99221 admissions.
What if providers had 95% level 3 admissions and 5% level 1 admissions? That would provide 570 level three admissions worth $190 each. Level 3 admissions would collect $108,300. This is about $33,000 more than the SHM/MGMA distribution would suggest, or a 44% increase in payments. This does not take into account alternative payer mix contributions. Remember, level 2 hospital admission documentation is different from level 3 documentation only in the medical decision making. Knowing how to document work already being provided is valuable in any practice.
RAC AUDITORS
Medicare may be targeting inappropriate payments to providers for hospital admissions. A practitioner's best defense against fraud accusations is to document thoroughly for work provided and to practice standard of care. Despite being an outlier, accurate stand alone documentation of medically necessary care should always support any coding distribution that results. I have thoroughly reviewed Medicare's Evaluation and Management Services Guide and can confirm that fear of an audit is not an element that should be used to guide coding decisions.