This 99224 CPT® lecture reviews the procedure code definition, progress note examples, distribution and RVU values for this relatively new subsequent observation care evaluation and management (E/M) code. CPT stands for Current Procedural Terminology. CPT® 99224 is the lowest (level 1) subsequent observation care code in this family of codes (99224, 99225 and 99226) and is part of the Healthcare Common Procedure Coding System (HCPCS). Observation care is considered outpatient care. A patient is considered outpatient until inpatient admission to a healthcare facility occurs. This procedure code lecture for subsequent observation care is part of a complete series of CPT® lectures written by myself, a board certified internal medicine physician with over ten years of clinical hospitalist experience in a large community hospitalist program. I have written my collection of evaluation and management (E/M) lectures over the years to help physicians and non-physician practitioners (nurse practitioners, clinical nurse specialists, certified nurse midwives and physician assistants) understand the complex criteria needed to stay compliant with the Centers for Medicare & Medicaid Services (CMS) and other third party insurance companies.
You can find my entire collection of constantly updated medical billing and coding CPT® lectures together in one place on my Pinterest site (CPT® lectures here and other associated E/M lectures here). You don't need to be a Pinterest member to get access to any of my CPT® procedure lectures. As you gain understanding of these E/M procedure codes, remember you have an obligation to make sure your documentation supports the level of service you are submitting for payment. The volume of your documentation should not be used to determine your level of service. The details of your documentation are what matter most. In addition, the E/M services guide says the care you provide must be "reasonable and necessary" and all entries should be dated and contain a CMS defined legible signature or signature attestation, if necessary.
The Centers for Medicare & Medicaid Services (CMS) has recognized subsequent observation care codes (99224-99226) since calendar year 2011's Physician Fee Schedule (PFS) with comment period (CMS-1503-FC). CPT® codes 99224-99226 should be used by the admitting physician for day(s) other than the initial or discharge date. Consulting physicians should continue to use established outpatient care codes 99211-99215 instead for all days other than the initial encounter, in most circumstances.
My interpretations discussed below are based on my review of the 1995 and 1997 E&M guidelines, the CMS E&M guide and the Marshfield Clinic audit point system for medical decision making. These resources can be found in my hospitalist resources section. The Marshfield Clinic point system is voluntary for Medicare carriers but has become the standard audit compliance tool in many parts of the country. You should check with your own Medicare carrier in your state to verify whether or not they use a different criteria standard than that for which I have presented here in my free educational discussion. I recommend all readers obtain their own updated CPT® reference book as the definitive authority on CPT® coding. I have provided access through Amazon to the 2015 CPT® standard edition pictured below and to the right. The American Medical Association (AMA) describes the 99224 CPT® procedure code as follows:
You can find my entire collection of constantly updated medical billing and coding CPT® lectures together in one place on my Pinterest site (CPT® lectures here and other associated E/M lectures here). You don't need to be a Pinterest member to get access to any of my CPT® procedure lectures. As you gain understanding of these E/M procedure codes, remember you have an obligation to make sure your documentation supports the level of service you are submitting for payment. The volume of your documentation should not be used to determine your level of service. The details of your documentation are what matter most. In addition, the E/M services guide says the care you provide must be "reasonable and necessary" and all entries should be dated and contain a CMS defined legible signature or signature attestation, if necessary.
99224 MEDICAL CODE DESCRIPTION
The Centers for Medicare & Medicaid Services (CMS) has recognized subsequent observation care codes (99224-99226) since calendar year 2011's Physician Fee Schedule (PFS) with comment period (CMS-1503-FC). CPT® codes 99224-99226 should be used by the admitting physician for day(s) other than the initial or discharge date. Consulting physicians should continue to use established outpatient care codes 99211-99215 instead for all days other than the initial encounter, in most circumstances.
My interpretations discussed below are based on my review of the 1995 and 1997 E&M guidelines, the CMS E&M guide and the Marshfield Clinic audit point system for medical decision making. These resources can be found in my hospitalist resources section. The Marshfield Clinic point system is voluntary for Medicare carriers but has become the standard audit compliance tool in many parts of the country. You should check with your own Medicare carrier in your state to verify whether or not they use a different criteria standard than that for which I have presented here in my free educational discussion. I recommend all readers obtain their own updated CPT® reference book as the definitive authority on CPT® coding. I have provided access through Amazon to the 2015 CPT® standard edition pictured below and to the right. The American Medical Association (AMA) describes the 99224 CPT® procedure code as follows:
Subsequent observation care, per day, for the evaluation and management of a patient, which requires at least two of these three key components: problem-focused interval history; problem-focused examination; medical decision making that is straightforward or of low complexity. Counseling and/or coordination of care with other clinicians or agencies is provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is stable, recovering, or improving. Physicians typically spend 15 minutes at the bedside and on the patient’s hospital floor or unit.
- History
- Physical Exam
- Medical Decision Making Complexity (MDM)
In addition to a face-to-face encounter, what are the absolute minimum requirements for this level one 99224 visit?
- Problem focused interval history: Requires only 1-3 components for the history of present illness (HPI) or documentation of the status of three chronic medical conditions. No past medical history or social history or family history or review of systems is required. Note, just one component of the HPI is required.
- Problem focused physical exam: Requires requires 1-5 organ systems (1997 guidelines). Three vital signs are considered one organ system. Therefore, documentation of just three vital signs meet criteria for a low level hospital follow up billing code. The CMS E&M guide on pages 31 and 32 describes the acceptable body areas and organ systems on physical exam.
- Straight forward or low complexity medical decision making (MDM): This is split into three components. The 2 out of the 3 highest levels in MDM are used to determine the overall level of MDM. The level is determined by a complex system of points and risk. What are the three components of MDM and the minimum required level of points and risk as defined by the Marshfield Clinic audit tool?
- Diagnosis (1 point)
- Data (0 points)
- Risk (minimal)
CLINICAL EXAMPLES OF CPT® 99224
With the purest interpretation of E/M rules in mind, what are some progress note documentation examples for a CPT® 99224, the level 1 subsequent observation care code? Although not required, many doctors use the subject, objective, assessment and plan (SOAP) note format for their documentation. A CPT® 99224 note could look like this:
In this example history (subjective) and physical (objective) meet the requirements to get paid for a 99224. Remember, the highest 2 out of 3 components determine the highest level of service for subsequent observation care visits. Do note that linking an ICD code to a CPT® code is required for all visits submitted for reimbursement from CMS. Therefore, most progress notes should provide at least one ICD code to clearly indicate a purpose for the visit. I suspect this is necessary to meet the reasonable and necessary threshold, unless that can be inferred from other chart documentation. Medicare doesn't want to pay for doctors to talk about the Superbowl with their patients. There must always be an approved ICD code linked with the CPT® code when billed to CMS.S) No pain (1 HPI)O) 120/80 80 Tmax 98.9 (three vital signs = one organ system)A) Nothing neededP) Nothing needed
I think it's always a good habit to include at least one ICD code, even though it's not technically required for E/M visits that can achieve compliance with history and physical components alone. Remember, the highest supported level of documentation for two out of three from history, physical and medical decision making on subsequent observation care visits will determine the appropriate level of service. For history, just one component of the HPI (character, onset, location, duration, what makes it better or worse etc.) or documentation of the status of three chronic medical conditions is required for this level one progress note. For physical exam, documentation of only one organ system is required and three vital signs counts as one organ system. That's not to say that a more thorough history or exam is not indicated. Only that E/M rules, if being graded by check marks for compliance, only require at least one bullet point for physical exam. Here is another clinical example of a SOAP note for a CPT® 99224 subsequent observation care:
S)NothingO) 120/80 80 Tm 98.6 (three vital signs = one organ system)A)HTN-stable, no changes planned.DM-stable, no changes planned (the status of three chronic medical conditions in place of HPI)COPD-stable, no changes plannedP) Nothing
As you know, documenting the status of three chronic medical conditions can be substituted for the HPI. With that said, you only need to document three vital signs for physical exam if nothing else is relevant and your documentation is complete and accurate for CPT® 99224. Note also, this documentation can support a CPT® 99224 code with no "proof" of a face-to-face encounter. One could document vital signs from home and never see the patient and meet the criteria for a CPT® 99224, in a checkbox kind of audit way. Medicare, however, only pays for face-to-face encounters on E/M visits. I do not recommend billing for CPT® 99224 without a face-to-face encounter and documentation should support that a face-to-face encounter took place should the visit ever get an audit. Here is another clinical example of appropriate documentation for a CPT® 99224:
S) Nothing neededO) 120/80 80 Tmax 98.6 (three vital signs = one organ system)A) 1) HTN, controlled (one point for diagnosis)P) Nothing needed
According to 1995 or 1997 guidelines, I can document a level one CPT® 99224 without ever asking the patient a question or laying hands on them, although, again, a face-to-face evaluation is always required. According to E/M guidelines, documenting the status of one chronic medical condition qualifies as low level risk in the decision making process. I have meet my requirements for 2 out of 3 areas by meeting requirements for physical exam (documenting three vital signs) and the decision making component (by documenting the status of one chronic medical condition). Remember, reasonable and necessary is always part of any evaluation.
There is a complicated table of risk that represents the last component of the decision making complexity and detailed on the CMS E&M guide linked through my hospitalist resource center above. What I have on my quick reference E/M coding card below only represents examples of moderate and high risk because one can achieve 99224 documentation requirements quite easily with minimal history and physical exam. I never use the risk table for a low observation follow-up progress note because I'm just not smart enough to memorize it. I only use the table of risk when determining moderate and high risk encounters. Here is another clinical example that meets documentation requirements for a CPT® 99224:
S)No Pain (one HPI)O)NothingA)HTN, no change (one point for diagnosis)P)Nothing
That's all you need folks. Documentation of two out of three areas at the lowest level needed. That means one HPI (no pain) and one physical exam (three vital signs) or one HPI (no pain) and low complex medical decision making (documentation of one stable medical problem such as HTN-stable), or documentation of physical exam (three vital signs) and low level medical decision making (HTN-stable).
Examples above represent the bare minimum required for a low level observation subsequent care visit in the hospital. This is not my patient population. That's why my total yearly level one documentation with CPT® 99224 is pretty low. Most patients in the hospital these days are much more complex than a level one of any service. Most hospital patients require an intensity of service much higher than a 99224. If a physician is frequently billing 99224, their patients should probably be at home surfing the internet and watching football.
DISTRIBUTION OF OBSERVATION SUBSEQUENT CARE CODES (99224-99226).
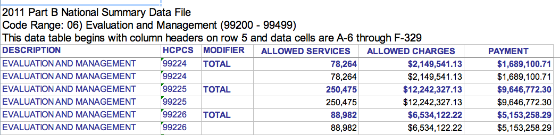
What is the distribution of CPT® code 99224 relative to other levels of service in this family of medical codes? CPT® group 99224-99226 is pretty new. CMS has only recognized these codes since 2011. However, CMS has data explaining how often 99224, 99225 and 99226 have been used. The graphic below was obtained from the 2011 CMS Part B National Procedure Summary Files data (2011 zip file) showing how many CPT® 99224 encounters were billed and the dollar value of their services for Part B Medicare. As you can see in the image below, E/M code 99224 was billed 78,264 times in 2011 with allowed charges of $2,149,541.13 and payments of $1,689,100.71.
RVU VALUE
How much money does a CPT® 99224 pay in 2016? That depends on what part of the country you live in and what insurance company you are billing. E/M procedure codes, like all CPT® billing codes, are paid in relative value units (RVUs). This complex RVU discussion has been had elsewhere on The Happy Hospitalist. For raw RVU values, a CPT® 99224 is worth 1.12 total RVUs. The work RVU for 99224 is valued at 0.76. Make sure to review the complete list of RVU values on common hospitalist E/M codes. What is the Medicare reimbursement for CPT® code 99224? In my state, a CPT® 99224 pays just over $41 in 2016. The dollar conversion factor for one RVU in 2014 is 35.8043.
My E/M reference card below has taught me that I should be billing for the work I'm providing and it has taught me how to document appropriately. You can see many more of my E/M lectures by clicking through on the provided link. If you need bedside help determining what level of care you have provided, I recommend reviewing the pocket card described below.
LINK TO E/M BEDSIDE POCKET REFERENCE CARD POST
|

Tweet


Tidak ada komentar:
Posting Komentar