This 99225 CPT® lecture reviews the procedure code definition, progress note examples, distribution and RVU values for this new since 2011 subsequent observation care evaluation and management (E/M) code. CPT stands for Current Procedural Terminology. CPT® 99225 is the middle (level 2) subsequent observation care code in this family of codes that also includes CPT® codes
99224 and
99226. All three codes are part of the Healthcare Common Procedure Coding System (HCPCS). Observation care is considered outpatient care. A patient is considered outpatient until inpatient admission to a healthcare facility occurs. This procedure code lecture for subsequent observation care is part of a complete series of CPT® lectures written by myself, a board certified internal medicine physician with over ten years of clinical hospitalist experience in a large community hospitalist program. I have written my collection of evaluation and management (E/M) lectures over the years to help physicians and non-physician practitioners (nurse practitioners, clinical nurse specialists, certified nurse midwives and physician assistants) understand the complex criteria needed to stay compliant with the Centers for Medicare & Medicaid Services (CMS) and other third party insurance companies.
You can find my entire collection of constantly updated medical billing and coding CPT® lectures together in one place on my Pinterest site (
CPT® lectures here and other associated
E/M lectures here).
You don't need to be a Pinterest member to get access to any of my CPT® procedure lectures. As you start to understand these E/M procedure codes, remember you have an obligation to make sure your documentation supports the level of service you are submitting for payment. The volume of your documentation should not be used to determine your level of service. The details of your documentation are what matter most. In addition, the E/M services guide says the care you provide must be "reasonable and necessary" and all entries should be dated and contain a CMS defined legible signature or signature attestation, if necessary.
99225 MEDICAL CODE DESCRIPTION
The Centers for Medicare & Medicaid Services (CMS) has recognized subsequent observation care codes (99224-99226) since calendar year 2011's Physician Fee Schedule (PFS) with comment period (
CMS-1503-FC). CPT® codes 99224-99226 should be used by the admitting physician for day(s) other than the initial or discharge date. Consulting physicians should continue to use established outpatient care codes 99211-99215 instead for all days other than the initial encounter, in most circumstances.
My interpretations discussed below are based on my review of the 1995 and 1997 E&M guidelines, the CMS E&M guide and the Marshfield Clinic audit point system for medical decision making. These resources can be found in my
hospitalist resources section. The Marshfield Clinic point system is voluntary for Medicare carriers but has become the standard audit compliance tool in many parts of the country. You should check with your own Medicare carrier in your state to verify whether or not they use a different criteria standard than that for which I have presented here in my free educational discussion. I recommend all readers obtain their own updated CPT® reference book as the definitive authority on CPT® coding. I have provided access through Amazon to the 2015 CPT® standard edition pictured below and to the right. The American Medical Association (AMA) describes the 99225 CPT® procedure code as follows:

 Subsequent observation care, per day, for the evaluation and management of a patient, which requires at least two of these three key components: an expanded problem-focused interval history; an expanded problem-focused examination; medical decision making of moderate complexity. Counseling and/or coordination of care with other clinicians or agencies is provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is responding inadequately to therapy or has developed a minor complication. Physicians typically spend 25 minutes at the bedside and on the patient’s hospital floor or unit.
Subsequent observation care, per day, for the evaluation and management of a patient, which requires at least two of these three key components: an expanded problem-focused interval history; an expanded problem-focused examination; medical decision making of moderate complexity. Counseling and/or coordination of care with other clinicians or agencies is provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is responding inadequately to therapy or has developed a minor complication. Physicians typically spend 25 minutes at the bedside and on the patient’s hospital floor or unit.
This medical billing code can be used to
bill based on time when certain requirements are met. However, documentation of time is not required to remain compliant with CMS regulations. If billed without time as a consideration, CPT® 99225 documentation should comply with the rules established by the 1995 or 1997 guidelines referenced above. The three important coding components for a subsequent observation care evaluation are:
- History
- Physical Exam
- Medical Decision Making Complexity (MDM)
Of note, the E/M coding requirements for CPT® 99225 are exactly the same as subsequent hospital care
CPT® 99232. For all subsequent observation care codes (99224-99226), the highest documented two out of three above components determines the correct level of service code. This is different from initial observation care encounter (99218-99220) rules, which require the highest documented three out of three above components.
In addition to a face-to-face encounter, what are the absolute minimum requirements for this level two 99225 visit?
- Expanded problem focused interval history: Requires 1-3 components for the history of present illness (HPI) or documentation of the status of three chronic medical conditions and one review of systems (ROS). No past medical history or family history or social history is required.
- Expanded problem focused physical exam:
- 1995 E/M guidelines require up to 7 systems or limited exam of affected body area and other symptomatic or related systems. Note the wordage difference with body systems or areas. They are not the same. The guidelines don't really clarify what "up to 7 systems" means so it's hard to justify exactly what that means. By this definition, just one system would qualify. I recommend instead to consider using the clearer 1997 guidelines.
- 1997 E/M guidelines require at least 6 bullets from one or more organ systems. A review of the acceptable "body areas" and "organ systems" can be found in the CMS E&M reference guide on pages 31 and 32.
- Moderate complexity medical decision making (MDM): This is split into three components. The 2 out of 3 highest levels in MDM are used to determine the overall level of MDM. The level is determined by a complex system of points and risk. What are the three components of MDM and the minimum required level of points and risk as defined by the Marshfield Clinic audit tool?
- Dignosis (3 points)
- Data (3 points)
- Risk (moderate). The table of risk can be found on page 37 of the CMS E&M reference guide.
The medical decision making point system is highly complex. I have referenced it in detail on my E/M pocket cards described below. These cards help me understand what level of service my documentation supports. I carry these cheat sheet cards with me at all times and reference them all day long. As a hospitalist who performs E/M services almost exclusively, these cards have prevented me from under and over billing thousands of times over the last decade.
CLINICAL EXAMPLES OF CPT® 99225
What are some progress note documentation examples for a CPT® 99225, the level 2 subsequent observation care code? Although not required, many doctors use the subject, objective, assessment and plan (SOAP) note format for their documentation. A CPT® 99225 note could look like this:
S) sharp pain in abd (1 HPI), no SOB (1 ROS)
O) 120/80 70 Tm 98.6 (three vitals is one organ)
Alert, abdomen soft, no guarding, bowel tones present, regular pulse, no wheezing, no leg edema, no rash (at least 6 bullets from at least one organ system)
A) Nothing needed
P) Nothing needed.
In this example history (subjective) and physical (objective) meet the requirements to get paid for a 99225. Remember, the highest 2 out of 3 components determine the highest level of service for subsequent observation care visits. Do note that linking an ICD code to a CPT® code is required for all visits submitted for reimbursement from CMS. Therefore, most progress notes should provide at least one ICD code to clearly indicate a purpose for the visit. I suspect this is necessary to meet the reasonable and necessary threshold, unless that can be inferred from other chart documentation. Medicare doesn't want to pay for doctors to talk about the basketball with their patients. There must always be an approved ICD code linked with the CPT® code when billed to CMS.
I think it's always a good habit to include at least one ICD code, even though it's not technically required for E/M visits that can achieve compliance with history and physical components alone. Remember, the highest supported level of documentation for two out of three from history, physical and medical decision making on subsequent observation care visits will determine the appropriate level of service. For history, at least one component of the HPI (character, onset, location, duration, what makes it better or worse etc.) or documentation of the status of three chronic medical conditions is required for this level two progress note. In addition, at least one review of systems is required as well. For physical exam, based on 1997 criteria, documentation of at least six bullets from one or more organ systems is required. Three vital signs counts as one organ system. That's not to say that a more thorough history or exam is not indicated. Only that E/M rules, if being graded by check marks for compliance, only require at least six bullet points for physical exam (when using 1997 guidelines). Here is another clinical example of a SOAP note for a CPT® 99225 subsequent observation care:
S) No SOB (1 ROS)
O) 120/80 70 Tm 98.6 (three vital signs as one organ system)
Alert, regular pulse, no wheezing, no leg edema, no rash (at least 6 bullets from at least 1 organ system)
A) HTN, stable, no changes planned
CAD, stable, no changes planned
P) Nothing needed.
This is a level 2 subsequent observation care progress note based on history and physical. The status of three chronic medical conditions substitutes for the HPI and meets the minimum requirement of one HPI. Add in one ROS and this is a level two history. The physical exam has at least six bullets from 1 organ system so this is a level two physical exam for subsequent observation care follow up. Note, while I have written the problems in my assessment, I am applying them to my HPI. CMS does not require SOAP notes. This is just how physicians are taught. I could write my note in essay form if I chose to do so. Sometimes, I apply the status of my three chronic conditions to apply to my data points too in MDM. They should apply because the documentation supports it. Here is another 99225 progress note based on history and MDM:
S) ROS not able secondary to delirium (highest level ROS by default). Patient has delirium since last night (1 HPI).
O) 120/80 70 Tm 98.6 (one bullet)
A) Left arm swelling consistent with cellulitis, new onset ( 3 points, new problem no workup)
P) Start antibiotics. (moderate risk for prescription drug management)
In this example, the ROS meets the highest level of care based on the explained inability to obtain a ROS. The HPI has at least one element (onset). This is a level two history. The physical exam, however, only meets criteria for a level one subsequent observation care visit because it only has one bullet (three vital signs). The MDM is moderate because it meets a level two for diagnosis based on the 3 points for a new problem with no workup planned. In addition, the risk table gives this moderate risk because of prescription drug management. Because this note has a level one physical, a level 2 MDM and a level 2 history, the highest two out of three elements of this note makes this a level two visit. See how easy that is? This is why my E/M bedside reference cards detailed below are so valuable. We do things every day that we under appreciate and under bill as a result. Remember, volume of the note does not matter. What's documented determines the level of service. Here is one final clinical example to review:
S) No CP (1 ROS)
O) Nothing
Hgb, 12.4 (1 point) ECG tracing personally reviewed shows chronic afib (2 points)
A) CAD, stable, no changes planned (1 point)
COPD, stable, no changes planned (1 point) (status of 3 chronic medical conditions)
Chronic Afib, stable, no changes planned (1 point)
P) No changes
This note meets a level two subsequent observation care progress note based on history and MDM. The status of three chronic medical conditions meets the criteria for a full HPI, more than enough for the required one HPI. With one ROS, this is a level two history. The physical exam offers nothing in this example. The MDM is moderate because it gets three points under the diagnosis component for describing established problems, stable or improved. The data portion gets three points, one point for reviewing lab and two points for personally reviewing the ECG. The risk table does not apply here. Remember, MDM is determined by the highest two out of three for diagnosis, data and risk.
I hope these common clinical examples offer further proof that documentation is key to staying compliant. Writing a novel is not required. As physicians, I think we tend to underestimate the level of complexity we encounter because we are used to it. We need to do a better job of documenting what we do and understand the rules we have been given to follow. Notice these notes are not long essays. They are strategically written to capture value in work we are doing but not describing in the correct manner. Don't be afraid to bill 99225 if the face-to-face encounter you provide is medically reasonable and necessary and your documentation supports CPT® 99225.
DISTRIBUTION OF OBSERVATION SUBSEQUENT CARE CODES (99224-99226).
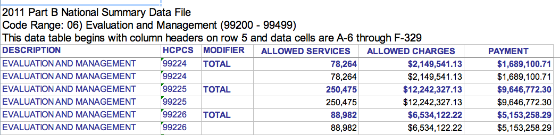
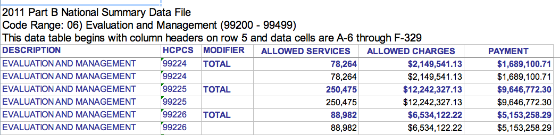
What is the distribution of CPT® code 99225 relative to other levels of service in this family of medical codes? The CPT® group 99224-99226 is pretty new. CMS has only recognized these codes since 2011. However, CMS has data explaining how often 99224, 99225 and 99226 have been used. The graphic below was obtained from the 2011 CMS
Part B National Procedure Summary Files data (
2011 zip file) showing how many CPT® 99225 encounters were billed and the dollar value of their services for Part B Medicare. As you can see in the image below, E/M code 99225 was billed 250,475 times in 2011 with allowed charges of $12,242,327.13 and payments of $9,646,772.30.
RVU VALUE
How much money does a CPT® 99225 pay in 2016? That depends on what part of the country you live in and what insurance company you are billing. E/M procedure codes, like all CPT® billing codes, are paid in relative value units (RVUs). This complex
RVU discussion has been had elsewhere on The Happy Hospitalist. For raw RVU values, a CPT® 99225 is worth 2.05 total RVUs. The work RVU for 99225 is valued at 1.39. Make sure to review the complete list of
RVU values on common hospitalist E/M codes. What is the Medicare reimbursement for CPT® code 99225? In my state, a CPT® 99225 pays around $70 in 2016. The
dollar conversion factor for one RVU in 2016 is 35.8043.
My E/M reference card below has taught me that I should be billing for the work I'm providing and it has taught me how to document appropriately. You can see many more of my
E/M lectures by clicking through on the provided link. If you need bedside help determining what level of care you have provided, I recommend reviewing the pocket card described below.