This 99205 CPT® lecture reviews the procedure code definition, progress note examples, RVU values, national distribution data and explains when this code should be used in the clinic and hospital setting. CPT stands for Current Procedural Terminology. This code is part of a family of medical billing codes described by the numbers 99201-99205. CPT® 99205 represents the high (level 5) office or other outpatient new patient visit and is part of the Healthcare Common Procedure Coding System (HCPCS). After you're done studying this lecture, make sure to also review the lectures on level three and level four new patient office visits. A patient is considered outpatient until inpatient admission to a healthcare facility occurs. This procedure code lecture for new office patient visits is part of a complete series of CPT® lectures written by myself, a board certified internal medicine physician with over ten years of clinical hospitalist experience in a large community hospitalist program. I have written my collection of evaluation and management (E/M) lectures over the years to help physicians and non-physician practitioners (nurse practitioners, clinical nurse specialists, certified nurse midwives and physician assistants) understand the complex criteria needed to stay compliant with the Centers for Medicare & Medicaid Services (CMS) and other third party insurance companies.
You can find my entire collection of medical billing and coding CPT® lectures together in one place on my Pinterest site (CPT® lectures here and other associated E/M lectures here). You don't need to be a Pinterest member to get access to any of my CPT® procedure lectures. As you gain understanding of these E/M procedure codes, remember you have an obligation to make sure your documentation supports the level of service you are submitting for payment. The volume of your documentation should not be used to determine your level of service. The details of your documentation are what matter most. In addition, the E/M services guide says the care you provide must be "reasonable and necessary" and all entries should be dated and contain a CMS defined legible signature or signature attestation, if necessary.
My interpretations discussed below are based on my review of the 1995 and 1997 E&M guidelines, the CMS E&M guide and the Marshfield Clinic audit point system for medical decision making. These resources can be found in my hospitalist resources section. The Marshfield Clinic point system is voluntary for Medicare carriers but has become the standard audit compliance tool in many parts of the country. You should check with your own Medicare carrier in your state to verify whether or not they use a different criteria standard than that for which I have presented here in my free educational discussion. I recommend all readers obtain their own updated CPT® reference book as the definitive authority on CPT® coding. I have provided access through Amazon to the 2015 CPT® standard edition pictured below and to the right. CPT® 99205 is an office or other outpatient procedure code and can be used by any qualified healthcare practitioner to get paid for their office or other outpatient new patient services. The American Medical Association (AMA) describes the 99205 CPT® procedure code as follows:
You can find my entire collection of medical billing and coding CPT® lectures together in one place on my Pinterest site (CPT® lectures here and other associated E/M lectures here). You don't need to be a Pinterest member to get access to any of my CPT® procedure lectures. As you gain understanding of these E/M procedure codes, remember you have an obligation to make sure your documentation supports the level of service you are submitting for payment. The volume of your documentation should not be used to determine your level of service. The details of your documentation are what matter most. In addition, the E/M services guide says the care you provide must be "reasonable and necessary" and all entries should be dated and contain a CMS defined legible signature or signature attestation, if necessary.
99205 MEDICAL CODE DESCRIPTION
My interpretations discussed below are based on my review of the 1995 and 1997 E&M guidelines, the CMS E&M guide and the Marshfield Clinic audit point system for medical decision making. These resources can be found in my hospitalist resources section. The Marshfield Clinic point system is voluntary for Medicare carriers but has become the standard audit compliance tool in many parts of the country. You should check with your own Medicare carrier in your state to verify whether or not they use a different criteria standard than that for which I have presented here in my free educational discussion. I recommend all readers obtain their own updated CPT® reference book as the definitive authority on CPT® coding. I have provided access through Amazon to the 2015 CPT® standard edition pictured below and to the right. CPT® 99205 is an office or other outpatient procedure code and can be used by any qualified healthcare practitioner to get paid for their office or other outpatient new patient services. The American Medical Association (AMA) describes the 99205 CPT® procedure code as follows:
Office or other outpatient visit for the evaluation and management of a new patient, which requires these three components: A comprehensive history; A comprehensive examination; Medical decision making of high complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient's and/or family's needs. Usually, the presenting problem(s) are of moderate severity. Physicians typically spend 60 minutes face-to-face with the patient and/or family.
This medical billing code can be used for time based billing when certain requirements are met. However, documentation of time is not required to remain compliant with CMS regulations. If billed without time as a consideration, CPT® 99205 documentation should comply with the rules established by the 1995 or 1997 guidelines referenced above. The three important coding components for an new patient office or other outpatient visit are the:
- History
- Physical Exam
- Medical Decision Making Complexity (MDM)
In order to appropriately code a level 5 (99205) new patient office visit, all three components (history, physical and MDM complexity) must achieve level five status. What are the absolute minimum requirements for this level five visit? These requirements are discussed below. In addition, as with all E/M encounters, a face-to-face encounter is always required. However, in the case of outpatient clinic codes, Medicare does allow incident to billing, where the the service is provided by someone other than the physician. If certain requirements are met, the physician may collect 100% of allowable charges in these situations. Services billed incident to are billed under the physician's provider number.
- Comprehensive history: Requires four or more elements of the history of present illness (HPI) OR documentation of the status of three chronic medical conditions. It also requires least one item each from past history (illnesses, operations, injuries, treatments), social history and family history. In addition, a complete review of systems is also required (10 or more organ systems) as well.
- Comprehensive examination: The CMS E&M services guide on pages 31 and 32 describes the acceptable body areas and organ systems for physical exam. Either a general multi-system examination or complete examination of a single organ system (with other symptomatic or related body area(s) or organ system(s) --1997 guidelines) is acceptable. For a general multi-system examination, 1997 guidelines require documentation of at least two bullets each in at least nine organs systems or body areas (described on pages 52-55 in E/M services guide) while 1995 guidelines require findings from about 8 or more of the 12 organ systems, not otherwise specified. Requirements for a complete single organ exam are discussed in the E/M services guide from pages 57-82.
- Medical decision making of high complexity (MDM): This is split into three components. The 2 out of 3 highest levels in MDM are used to determine the overall level of MDM. The level is determined by a complex system of points and risk. What are the three components of MDM and what are the the minimum required number of points and risk level as defined by the Marshfield Clinic audit tool?
- Diagnosis (4 points)
- Data (4 points)
- Risk (high); The risk table can be found on page 37.
CLINICAL EXAMPLES OF CPT® 99205
What are some progress note documentation examples for a CPT® 99205, the level 5 new patient visit in an office or other outpatient setting? Although not required, many doctors use the subject, objective, assessment and plan (SOAP) note format for their documentation. A CPT® 99205 note could look like this:
In this example, the history (subjective), physical (objective) and MDM (assessment and plan) components all meet the minimum requirements to get paid for a 99205 new patient outpatient clinic visit based on the definition of this CPT® code detailed above. Both the history and physical are comprehensive. Medical decision making is high complexity because two of the three components in MDM meet the threshold for overall high complexity. Diagnosis is 4 points (high complexity), data is 4 points (high complexity) and risk is moderate based on an undiagnosed new problem with uncertain prognosis or acute illness with uncertain prognosis. Since two out of three are at least high, the overall MDM is high. Choosing high risk is appropriate because two out of three components of MDM did reach high complexity status based in the E/M rules.Subjective: Abdominal pain. RLQ. Started yesterday. Constant. 3/10. Associated fever yesterday now resolved (at least 4 HPI). No nausea, chest pain, dizziness, shortness of breath. In the absence of these pertinent positives and negatives, all other ROS were reviewed and were otherwise negative (at least 10 ROS ). Nonsmoker. No personal history of colitis. No family history of colitis. (at least one element each from 3 of 3 past history, social and family)Objective: 120/80 80 Tmax 98.9 (three vital signs = one bullet) alert, memory intact, no acute distress, no icterus, pupils symmetric, poor dentition, oropharynx normal, no thyroid masses, trachea midline, no neck adenopathy, no groin adenopathy, normal respiratory effort, normal breath sounds, normal heart tones without murmur or JVD, no leg edema, positive bowel tones, no guarding RLQ, no palpable masses or organomegally, no skin rashes, no induration. (at least 2 bullets each in nine areas/systems)Assessment: 1) Abdominal Pain RLQ (4 points for diagnosis, new problem, more work-up planned)Plan: Check CBC, CT scan abdomen today. (2 points for data, one point each for ordering lab and radiology). I discussed case details personally with Dr XYZ regarding the potential need for surgical consultation. They will evaluate in their office after the CT is performed. (2 points for data).
Remember, the code group (99201-99205) requires all three elements (history, physical, MDM) to meet the minimum level of service as opposed to the outpatient established code group (99211-99215) which has the two out of three requirement. Stated another way, the lowest level of documentation from history, physical and MDM will determine the overall appropriate level of service for new clinic patient evaluations. If the MDM and physical meet criteria for 99205 but the history only meets the criteria for a 99203 visit, then 99203 is the correct code to choose for the visit. Taken to the extreme, if the MDM and the physical exam both meet criteria for 99205 but the history only meets the criteria for a 99201 evaluation, then the correct code to choose is 99201. Here is another example of an appropriately coded 99205 new patient office visit:
As you know, documenting the status of three chronic medical conditions can substitute for the HPI. Add in at least 10 additional review of systems and one element each from past history, family and social elements and the minimum history documentation required for CPT® 99205 has been met. The physical exam meets the comprehensive requirement with at least two bullets in each of nine areas or systems. All physical exam components offer value to the encounter to exclude potential complications of therapy or to search for evidence of decompensated disease.History: Cough resolved last week after stopping ACE inhibitor. No SOB. No CP. Complains of headache 7/10 started yesterday. All other systems reviewed and negative. (10 ROS allowed due to this notation) History of COPD present. Smoking, no interest in quitting. No FH of lung cancer. (one element each from past history, family and social)Physical Exam: 210/90 90 Tmax 98.9 (three vital signs = one bullet) alert, memory intact, no acute distress, no icterus, pupils symmetric, poor dentition, oropharynx normal, no thyroid masses, trachea midline, no neck adenopathy, no groin adenopathy, normal respiratory effort, normal breath sounds, no crackles or wheezes, normal heart tones without murmur, no JVD, no leg edema, positive bowel tones, no guarding, no palpable masses or organomegally, no skin rashes, no induration, no weakness on neurological exam. (at least 2 bullets each in nine areas/systems)Assessment: HTN-worse with numbness and headache. Suspect malignant HTN. See med changes.DM-stable, no changes planned.COPD with resolved cough-stable, no changes planned. (the status of three chronic medical conditions in place of HPI) (4 points for diagnosis- see discussion below)Plan: Give dose of clonidine now. Start ARB for HTN. (moderate risk for prescription drug management). Go to the ER to rule out head bleed. Consider admission to hospital.
The MDM is high complexity. This progress note documentation gets four diagnosis points for a new problem (headache) with more work up planned. In addition, this represents high risk on the risk table for chronic illness (HTN) with severe exacerbation, progression or side effects. The data component of medical decision making is irrelevant as only two out of three components for MDM require high complexity status within MDM. These complexities are displayed on my bedside E/M reference card shown below. The highest two out of three components for MDM are of high complexity and therefore this overall documentation supports CPT® 99205. Below is another example of a new patient 99205 office visit:
S: HA present 3/10, for 3 days and constant. Associated with double vision (at least 4 HPI) No fever, no neck stiffness, no nausea/vomiting. No chest pain or SOB. All other systems reviewed and negative. (at least 10 ROS based on this notation) No history of migraines. Nonsmoker. No FH brain cancer. (one element each from past history, social and family elements)This new patient outpatient evaluation is appropriate for CPT® 99205 as the history, physical and MDM all contain the necessary documentation based on the Marshfield Clinic audit tool. Medical decision making is high because the diagnosis element is high complexity (4 points for new diagnosis with more work-up planned) and the data element is high complexity (4 points for ordering lab, MRI and discussing the case). A risk table assessment is not necessary as high complexity is already defined. Therefore, the highest two out of three elements in MDM are high. Here is another progress note example of a level 5 new patient office visit:
O: 120/80 90 Tmax 98.9 (three vital signs = one bullet), no head trauma, alert, memory intact, no acute distress, no icterus, pupils symmetric, EOMI, poor dentition, oropharynx normal, no thyroid masses, trachea midline, no neck adenopathy, no groin adenopathy, normal respiratory effort, normal breath sounds, no crackles or wheezes, normal heart tones without murmur, no JVD, no leg edema, positive bowel tones, no guarding, no palpable masses or organomegally, no skin rashes, no induration, normal neurological exam. (at least 2 bullets each in nine areas/systems)
A: Acute HA wit double vision. No history of chronic headaches (one new problem with more work up planned and of uncertain prognosis is 4 points on MDM for diagnosis)
P: Check CBC/BMP. I called the neurologist and personally discussed case details with them today. They recommended an MRI today and to follow up in their office after it's done in the next day or two. (4 points for date with 1 point for lab, 1 point for MRI and 2 points for discussing case with another healthcare provider).
S: 48 year old male here to establish care. /SOB/N/V/HA. No neuropathy. No polyuria or polydypsia. Average blood sugar reading 145. Occasional chest pain with exertion. Better with rest. Good exercise tolerance. All other systems reviewed and negative. (at least 10 ROS based on this notation) Nonsmoker. No family history of CAD. Diabetes type II for 10 years. (one element each from past history, family and social elements)Both the history and physical meet minimum criteria for CPT® 99205 with comprehensive requirements documented for both. Medical decision making is high based on a 4 points for both the diagnosis and data components. The moderate risk table assessment does not apply. Remember, the highest two out of three elements from data, diagnosis and risk determines the overall level of MDM complexity.
O: 120/80 90 Tmax 98.9 (three vital signs = one bullet), no head trauma, alert, memory intact, no acute distress, no icterus, pupils symmetric, poor dentition, oropharynx normal, no thyroid masses, trachea midline, no neck adenopathy, no groin adenopathy, normal respiratory effort, normal breath sounds, no crackles or wheezes, normal heart tones without murmur, no JVD, no leg edema, positive bowel tones, no guarding, no palpable masses or organomegally, no skin rashes, no induration, normal neurological exam. (at least 2 bullets each in nine areas/systems)
A: 1) HTN, controlled, no changes planned. 2) DM II, uncontrolled. 3) CAD, with stable angina. 4) COPD stable no changes planned. (4 points on MDM for diagnosis and substituting three chronic medical conditions for HPI)
P: Increase Metformin from daily to BID dosing. (moderate risk for prescription drug management). Order Echo (1 point in data for ordering echo). Check CBC (1 point in data for ordering lab). EKG done. Tracing personally reviewed. No ST or TW changes at rest. Sinus rhythm ( 2 points in data for independent visualization of tracing).
USING NEW PATIENT CLINIC CODES IN THE HOSPITAL SETTING
The CPT® medical billing code group 99201-99205 should used by Hospitalists and other physicians or non-physician practitioners in the hospital setting under certain circumstances. I have previously discussed all the possible initial encounter codes that could be used in the hospital setting. These new patient clinic and other outpatient visit codes are included as possibilities. I have provided a detailed discussion of that decision tree analysis at the link provided just above. However, I will discuss the pertinent portions of that analysis here.
For patients admitted observation status, the attending physician should choose from the observation group of medical codes 99218-99220 for the initial encounter, 99224-99226 for observation status follow-up codes, and 99217 for observation discharge. Under certain situations, same day admit and discharge billing codes 99234-99236 or critical care procedure codes may also apply too. This is not the case for consultants taking care of observation status patients. What codes should a consultant use in an observation status situation? This is where the correct code decision can get very complicated. Medicare no longer recognizes consult procedure codes. Consultants should pick the appropriate level of service from the new outpatient clinic code group 99201-99205 as their initial encounter, but only IF the patient has NOT been seen previously by the physician or a physician partner of theirs in the same group and exact same specialty and subspecialty within the previous three years. Alternatively, critical care codes can be used instead if documentation supports their use.
If the patient HAS been seen in the last three years by the same physician or partner physician in the same group and exact same specialty and subspecialty, the consultant should use the established patient clinic code group 99211-99215 on their initial date of service and continue to use that code group for all subsequent observation services, including the day of discharge. Remember, all hospital observation CPT® code groups are reserved only for the attending physician. If a patient qualifies as a new patient but clinician documentation does not support any code from the code group 99201-99205 (usually because of the three out of three documentation requirement), then it is appropriate to instead choose a code from the established patient code group (99211-99215) that meets documentation requirements. This guidance has previously been confirmed by Medicare carriers.
The above discussion relates to Medicare because Medicare does not accept consult codes. Other insurances may still accept consultation codes. In those cases, the consultant should chose a level of service from medical code group 99241-99245 (outpatient consult codes) as the initial encounter and then pick a billing code from the established patient clinic codes 99211-99215 for all subsequent care visits, including the day of discharge, while the patient is hospitalized for observation services. If the patient is formally admitted inpatient, the consultant should use the inpatient subsequent care codes 99231-99233 for all subsequent face-to-face encounters.
DISTRIBUTION OF NEW PATIENT OFFICE OR OTHER OUTPATIENT VISIT CODES (99201-99205)
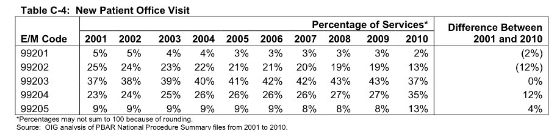
What is the distribution of CPT® code 99205 relative to other levels of service in this medical code group? The chart below was published in May, 2012 by the OIG in a report titled Coding Trends of Medicare Evaluation and Management Services on page 21. As you can see, between 2001 and 2010, the distribution of new patient office visits 99204 and 99205 has shifted higher (an increase of 12% and 4% respectively) while the proportion of level three 99203 has remained constant with no change from 2001-2010. In 2010, CPT® code 99205 represented 13% of all services from code group 99201-99205.
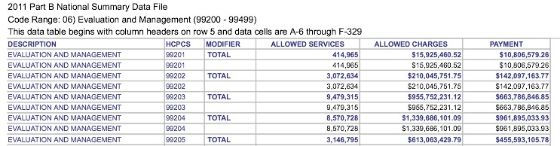
Here is data from the most recent 2011 CMS Part B National Procedure Summary Files data (2011 zip file) showing how many CPT® 99205 encounters were billed and the dollar value of their services for Part B Medicare. As you can see in the image below, E/M code 99205 was billed 3,146,795 times in 2011 with allowed charges of $613,063,429.79 and payments of $455,593,105.78.
RVU VALUE
How much money does a CPT® 99205 pay in 2016? That depends on what part of the country you live in and what insurance company you are billing. E/M procedure codes, like all CPT® billing codes, are paid in relative value units (RVUs). This complex RVU discussion has been had elsewhere on The Happy Hospitalist. For raw RVU values, a CPT® 99205 is worth 4.77 total RVUs for facility services and 5.82 total RVUs for non-facility. The work RVU for 99205 is valued at 3.17. A complete list of RVU values on common hospitalist E/M codes is provided at the provided link. What is the Medicare reimbursement for CPT® code 99205? In my state, a CPT® 99205 pays just under $160 (facility) and just over $193 (non-facility) in 2016. The dollar conversion factor for one RVU in 2014 is $35.8043.
My coding card taught me that I should be billing for the work I'm providing and it has taught me how to document appropriately. You can see many more of my E/M lectures by clicking through on the provided link. If you need bedside help determining what level of care you have provided, I recommend reviewing the pocket card described below.
LINK TO E/M BEDSIDE POCKET REFERENCE CARD POST
|

Tweet


Tidak ada komentar:
Posting Komentar