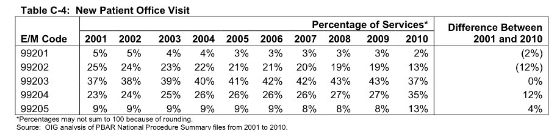
Why is this important? Because the assumption of physician fraud is alive and well. One of the report's stated objectives was to "to identify and describe physicians who consistently billed higher level E/M codes in 2010". The Centers for Medicare & Medicaid Services (CMS) has started sending letters to physicians with outlying billing patterns defined by computer algorithms. If you are a physician who consistently bills at a higher level than your colleagues, you may get correspondence from the Centers for Medicare & Medicaid Services detailing these concerns. The complex rules of E/M medicine are not routinely taught with urgency to training or practicing physicians. This leaves untrained physicians guessing how to choose the correct E/M code. The best defense a physician can mount is to accurately submit E/M charges based on what their medically necessary documentation supports. I have provided many of these coding rules in detail on my bedside cheat sheet pocket card previewed below.
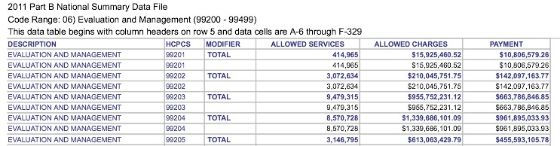
If you want to know which E/M codes the Recovery Audit Contractors (RAC) are likely reviewing, I think it's important to know which E/M codes are most commonly being used. This CMS website provides access to yearly updated Excel files containing Medicare Part B National Summary File data. Each of these yearly titled zip folders contain a file with information on allowed services, allowed charges and payments for all E/M CPT® codes. As of this publication, the most recent E/M information is provided in the Y2011_99201.xls file embedded within this 2011 file folder. I think this data gives a good idea of the most often used E/M codes by clinicians. While these files don't include E/M data by physicians billing to non-Medicare insurance companies, I think it's safe to assume this CMS data provides a large enough sample size to make assumptions on the top 10 most frequently used E/M codes. I have reviewed the file data and created these tables below for reference.
| 2011 | CPT® code | Allowed services | Allowed charges ($) | Payments ($) |
| 1 | 99213 | 100,268,652 | 6.8 billion | 4.7 billion |
| 2 | 99214 | 81,310,974 | 8.2 billion | 5.7 billion |
| 3 | 99232 | 50,949,134 | 3.6 billion | 2.8 billion |
| 4 | 99233 | 22,285,570 | 2.3 billion | 1.8 billion |
| 5 | 99212 | 18,501,855 | 745 million | 530 million |
| 6 | 99231 | 12,406,607 | 480 million | 380 million |
| 7 | 99223 | 11,771,925 | 2.3 billion | 1.8 billion |
| 8 | 99285 | 9,879,784 | 1.7 billion | 1.3 billion |
| 9 | 99215 | 9,694,388 | 1.3 billion | 940 million |
| 10 | 99308 | 9,636,112 | 620 million | 460 million |
| 2011 | CPT® code | Allowed charges ($) | Payments($) | Allowed Services |
| 1 | 99214 | 8.18 billion | 5.71 billion | 81,310,974 |
| 2 | 99213 | 6.79 billion | 4.71 billion | 100,268,652 |
| 3 | 99232 | 3.57 billion | 2.84 billion | 50,949,134 |
| 4 | 99223 | 2.31 billion | 1.81 billion | 11,771,925 |
| 5 | 99233 | 2.25 billion | 1.79 billion | 22,285,570 |
| 6 | 99285 | 1.67 billion | 1.30 billion | 9,879,784 |
| 7 | 99204 | 1.34 billion | 962 million | 8,570,728 |
| 8 | 99215 | 1.32 billion | 935 million | 9,694,388 |
| 9 | 99291 | 1.12 billion | 884 million | 5,045,749 |
| 10 | 99222 | 1.00 billion | 784 million | 7,506,127 |
Based on allowed charges and payment, the most expensive E/M service is the level 4 established patient clinic code (99214). Three new codes make the top ten list based on allowed charges and payments. They are the initial critical care code (99291), the level four new patient clinic code (99204) and the level 2 initial inpatient hospital evaluation code (99222). When based on allowed charges, three of the most common E/M codes based on frequency of allowed services fall off the list. They are the level two established patient office visit (99212), the level one inpatient hospital subsequent care code (99231) and nursing home code 99308.
The Happy Hospitalist provides a great resource for learning many of these most frequently billed E/M codes as well as guidance on many frequently encountered clinical scenarios that involve coding confusion. You can find the entire collection of E/M coding information in the evaluation and management resource area. In addition, the E/M pocket reference card detailed below provides guidance on how to approach E/M decision making at the bedside. You can also find a wealth of other information in the hospitalist resource area as well..
LINK TO E/M POCKET CARD POST
|
Tweet