We strongly encourage the General Assembly to accept new federal Medicaid funding that will be made available to Illinois in 2014 to fill a historic gap in the Medicaid program and provide health care coverage for hundreds of thousands of the lowest income uninsured Illinois residents. The measure will strengthen the financial health of our hospitals and other health care providers and boost our local economies as federal funds create jobs.
Medicaid has never covered all low-income individuals. It has always had a gap. Even if you are very poor, you do not qualify for Medicaid unless you are also elderly, disabled, pregnant, parenting or a minor child. Eliminating this gap in Medicaid opens the door for coverage to people with income under $16,000 who are ages 18-65, not officially disabled and not raising a minor child. For example, vital health coverage would be available to young adults just coming out of high school or college and starting their working lives; other young adults experiencing underemployment after a tour in the military (Illinois has 43,000 uninsured veterans); older adults whose children have passed age 18 who are not high earners; and people troubled with mental health and other issues that block their efforts at employment.
The State of Illinois, its localities, and all of the rest of us have been filling this Medicaid gap. We do it through charity care programs, safety net healthcare arrangements funded by property taxes, and state-funded human services programs that could be covered by Medicaid if the individual were eligible. The average U.S. family and their employers pay an extra $1,000 in health insurance premiums each year to compensate for health care for the uninsured. The Kaiser Family Foundation estimates that total uncompensated care in Illinois will decline by approximately $953 million from 2013 - 2022. Townships and General Assistance providers will be relieved from paying for coverage of those who are uninsured and are currently ineligible for Medicaid.
The brunt of the Medicaid gap also falls on those not covered – poor health, premature death, lowered employability and productivity, lost opportunity, medical bankruptcy and more. SB 26 will allow the State of Illinois to use federal funds to close the Medicaid coverage gap, address these health inequities, and begin to address the problem of rising health care costs due to uncompensated care for the uninsured.
The Federal government will provide 100 percent of the cost of filling the Medicaid gap for the first three years ($4.6 billion for the Illinois economy), and 90 percent of the cost after that ($21 billion over the first ten years). This means nearly 20,000 new jobs, which means paychecks being spent in stores and restaurants. The tax revenue resulting from this federal investment in our state’s health care system will more than cover the state’s small financial contribution.
In announcing that she would accept the federal money to fill the Medicaid gap in her state, Arizona’s Governor Jan Brewer simply said, “I did the math”. Seven Republican governors, all at one time vocal opponents of the measure, have now joined this pragmatic and sensible chorus. It is just too obviously in the best interests of their people and their states to reject.
Health care coverage keeps people healthier and reduces overall health system costs. That’s why we, the undersigned organizations – a diverse constituency of consumers, providers, hospitals, local governments, businesses and insurance companies throughout the state – support SB 26 and urge the Illinois General Assembly to pass this bill.
Signed,
AARP Illinois
Aetna, Inc.
AIDS Foundation of Chicago
Heartland Alliance for Human Needs & Human Rights
Illinois Hospital Association Illinois Maternal and Child Health Coalition
Illinois Primary Health Care Association
Meridian Health Plan of Illinois
Sargent Shriver National Poverty Law Center
SEIU Healthcare Illinois Indiana
Dual Eligibles Next to Move into Managed Care in Illinois
On February 22, the U.S. Department of Health and Human Services announced a Memorandum of Understanding (MOU) with the state of Illinois for a demonstration project that will enroll approximately 136,000 dual eligibles in northeastern and central Illinois into managed care plans. (“Dual eligibles” are individuals who have coverage through both Medicare and Medicaid.) Illinois is the fourth state to receive an MOU for this demonstration, known nationally as the Medicare Medicaid Financial Alignment Initiative (MMAI).
AgeOptions and other organizations that serve older adults have been following the development of this new project, as it will significantly affect the lives of our clients. Here is what we have learned about this new initiative from our research and communications with the entities involved, including the Illinois Department of Healthcare and Family Services and various managed care organizations:
The MMAI project is part of a national effort to better coordinate care for dual eligible beneficiaries. Dual eligibles tend to be sicker and cost more than other Medicare and Medicaid beneficiaries. To address this, as part of the Affordable Care Act, the Centers for Medicare and Medicaid Services created a Medicare-Medicaid Coordination Office (MMCO) to “make sure Medicare-Medicaid enrollees have full access to seamless, high quality health care and to make the system as cost-effective as possible.” One of the MMCO’s first projects has been working with states to implement initiatives to coordinate care for dual eligibles.
Currently, dual eligibles must navigate and manage multiple systems of coverage in order to access the health care they need (Medicare, Medicare Part D prescription drug plans, and Medicaid). This can be very complex and taxing for individuals who have multiple complex health needs. Therefore, the goals of the MMAI project are to simplify this process and provide higher quality and more coordinated care for dual eligibles.
In January 2014, dual eligibles in the greater Chicago area and parts of Central Illinois will be enrolled into managed care plans. These plans must provide care managers and other supports to coordinate their members’ care, in addition to paying for members’ medical services and long term services and supports (LTSS). In exchange, these plans will be paid a capitated rate by the state of Illinois and CMS. (“Capitated rate” means the plans will receive a flat rate for each member that they serve, instead of being paid for each individual service that a member receives.) The inclusion of long term services and supports in this project is significant, as these services may be ‘new territory’ to some managed care organizations. In addition to providing coverage for LTSS provided in long term care facilities, MMAI plans will be responsible for covering home and community based services, such as the Community Care Program. This may cause confusion for dual eligible beneficiaries who are used to receiving Community Care Program services through the existing system, so agencies working with older adults will have to provide education and assistance to help our clients understand these new changes.
Illinois has selected eight managed care plans to provide MMAI coverage. Those eight plans are:
- Chicago area: Aetna Better Health, Blue Cross/Blue Shield of Illinois, HealthSpring, Humana, IlliniCare (Centene), and Meridian Health Plan of Illinois
- Central Illinois: Molina Healthcare, Health Alliance
Counties that will be part of the MMAI project:
- Greater Chicago area: Cook, DuPage, Lake, Kane, Kankakee, and Will counties
- Central Illinois: Christian, Champaign, DeWitt, Ford, Knox, Logan, Macon, McLean, Menard, Peoria, Piatt, Sangamon, Stark, Tazewell, and Vermilion counties
For more information about the Illinois MMAI project, please see the following resources:
CMS fact sheet
Illinois Memorandum of Understanding
Illinois Department of Healthcare and Family Services webpage on Illinois Care Coordination Initiatives (see section on MMAI)
For Better Healthcare Join The Small Business Healthcare Consoritum
Our changing health care system will have a profound effect on all of us. Now that the election is over and the Supreme Court has ruled, the Affordable Care Act (ACA) is not going away. It will not be repealed and it is up to us to make sure it will work for small businesses and individuals as it was intended to do.
That’s why I joined the Campaign for Better Health Care’s newly created Small Business Health Care Consortium (SBHCC). This consortium views the needs of small businesses and their employees as a top priority.
And, as a member of the Steering Committee of the SBHCC I am personally inviting you to join our network of small businesses who know that only through our collective voices that will assure that the Affordale Care Act live up to its goal of making healthcare affordable for all.
Discussions around health reform have been confusing and, sometimes, even misleading. It is the goal of the SBHCC to provide factual information about the changes that are already happening and those coming in the near future. The SBHCC discusses the benefits and opportunities of the ACA and what Illinois small businesses need to do to make sure this law will benefit them.
Many key components of the ACA are national in nature. For instance, small businesses currently providing health insurance to their employees could be eligible for a 35% tax credit. And, while employers with fewer than 50 full time employees are not required to provide health insurance, their employees can take advantage of the ACA’s benefits.
Other components will be implemented at the State level and these decisions will either enhance small businesses or provide another hurdle. One important component is that all states must implement a health insurance exchange (marketplace). These exchanges will include a rate review process with defined, easy to understand plans to consider and review side-by-side.
As small business owners we share many of the same, serious business challenges. It is my hope that you and your small business peers do want to learn more about the ACA. Let’s take this opportunity to act collectively to get control of health insurance costs and improve access to coverage. The opportunity to create positive change is now. It is about fairness and choices for small businesses. To that end I like for you to hear my own personal story about how the new healthcare law will effect me.
Howard Lee
CIO
Wirehead Technology
The Negative Impact of SMART Act Cuts
IPXP To Stop Accepting Applications March 2nd
The federal office charged with implementing health care reform announced last Friday that the subsidized plans that are currently insuring more than 100,000 individuals nationwide, will be closing their doors to new enrollees months before other coverage is available on the new insurance exchanges.
Although most of the provisions of the Affordable Care Act do not become effective until January 1, 2014, the law set up interim plans, called “Pre-Existing Condition Insurance Plans” for people who could not buy health insurance on the private market because of serious health conditions, including HIV. In Illinois, the state opened the Illinois Pre-Existing Insurance Plan (IPXP) in August 2010. Approximately 3000 people now have insurance though IPXP. Although those people currently enrolled in those plans will continue to have coverage until January 1, 2014, when they will be able to move to private insurance coverage, Friday’s announcement means that no new applications will be accepted after March 2, 2013.
Ann Fisher, Executive Director of the AIDS Legal Council of Chicago, explained why this is bad news for people with HIV or any other pre-existing condition that blocks them from getting private insurance. “IPXP has been an important source of health care coverage for people with HIV, including people on the AIDS Drug Assistance Program whose income climbs above 300% of the federal poverty level (about $35,000) but do not have health insurance on the job and cannot afford to pay for their medications themselves. “
The state has been able to refer those individuals to IPXP, and to help pay the IPXP premiums, so that they do not lose access to their medications. Fisher explained that IPXP was always meant to be a temporary program, set to expire once pre-existing conditions no longer prevent people from buying insurance. “But,” she added “we always assumed, perhaps naively, that IPXP would continue to accept new enrollees until very close to January 1st.” “It appears,” she added,” that IPXP is a victim of its own success. There was a limited pool of money available for the plans, and in order to make sure they can continue to pay claims of current enrollees, they now have to cut off future ones.”
The AIDS Legal Council is trying to get out the word about the closing of enrollment, and encouraging anyone who has been without insurance for at least six months to quickly apply for IPXP. ALCC is available to answer questions or assist with the enrollment process. They can be reached at 312-427-8990.
Ann Fisher
AIDS Legal Council of Chicago
ann@aidslegal.com
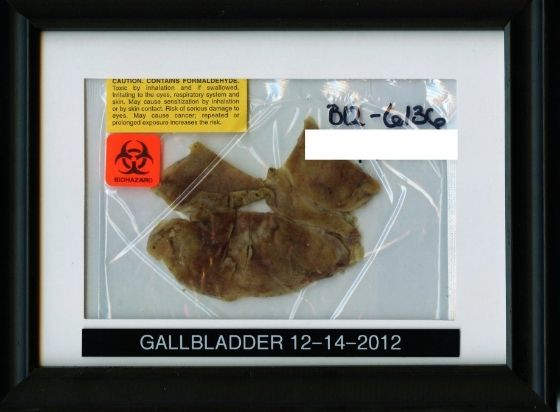
How To Dispose of Medical Waste? Take It Home and Frame It! (Picture)
If you ask me, this guy must have been stoned when he did this. Or maybe he just bagged his common sense when he decided to hang toxic medical waste as a show piece in his living room. Why not just let the hospital dispose of it like everyone else? Let's think about the possibilities, shall we? Perhaps he's part of a growing movement of environmentalists trying to reduce their carbon foot print by keeping their medical waste from ending up in the local landfill. I don't know how common it is for people to request their own body parts or other waste after surgery. For some folks, saving their surgical waste might be a fetish. Remember, there are folks who like to cut off their balls. Heck, this might even be a reality TV series some day. For others, it might be the cool factor. And for others yet, they may want to keep their body parts for religious reasons.
I heard a story once about an elderly woman who had to have both of her legs amputated after a freak car accident. She requested both her legs be given back to her after surgery so they could be placed in the coffin with her body upon her death. Where do you store human legs while waiting to die? Why, with the leg-of-lamb, of course. What was the reason for wanting to keep the legs? She wanted to make sure she had a leg up on everyone once she got into Heaven. Personally, I suspect she wanted to make one of those leg lamps
As for our guy with the gallbladder, whatever his motivation for saving his toxic organic waste, you have to admire him for being bold. How many of you would frame your sack for all your friends and family to see?

This post is for entertainment purposes only and likely contains humor only understood by those in a health care profession. Read at your own risk.
Tweet
IRS Issues Guidance on Health Insurance Premium Tax Credit - Clarification
The IRS issued a final regulations on when an employer-sponsored plan is considered "affordable" for an individual related to the employee for purposes of eligibility for a premium tax credit. Under Health Care Reform, employees may be eligible for a premium tax credit to purchase health insurance through the future health insurance exchanges if, among other reasons, the employer plan is deemed unaffordable.
The final regulations clarify that for taxable years beginning before January 1, 2015, an eligible employer-sponsored plan is affordable for related individuals if the portion of the annual premium the employee must pay for self-only coverage does not exceed 9.5% of the taxpayer's household income.
An employer plan will be affordable for family members if the cost of self-only coverage does not exceed 9.5% of the employee's household income. In other words, for purposes of whether family members are eligible for tax credits, the affordability of family coverage is not taken into account; all that matters is that the cost of self-only coverage is affordable to the employee
For purposes of applying the affordability exemption from the individual mandate in the case of related individuals, the required contribution is based on the premium the employee would pay for employer-sponsored family coverage.
For an employee eligible under an employer plan, affordability (for individual mandate exemption purposes) will be based on whether the cost of self-only coverage exceeds 8% of the employee's household income. For a related individual (such as a spouse or child), however, affordability for this purpose will be based on whether the cost of family coverage exceeds 8% of household income. Under these rules, members of an employee's family may qualify for an individual mandate exemption, even though the offer of affordable employer coverage to the employee would require the employee to enroll or risk paying a penalty.
These final regulations apply to taxable years ending after December 31, 2013.
For a copy of the final regulations, please click here.
This post originally appeared on February 5, 2013, on the Robert Slayton & Associates, Inc. blog. By Larry Grudzien, Attorney-At-Law
The HHS Secretary Visits Chicago
.JPG) |
| Secretary Sebelius speaks to a full house at the Chicago Cultural Center |
On Thursday, Sec. Sebelius spoke at the Chicago Cultural Center. Preceding her was Bechara Choucair, Commissioner of the Chicago Department of Public Health, who presented an overview of the Healthy Chicago program and its impact thus far. Sebelius delivered a call to action to those in attendance, citing the need for affordable, accessible health insurance for all as a crucial step in the national public health strategy. With only eight months before the state health marketplace is open for enrollment, and ten months before it is fully operational, promoting awareness of the health insurance exchange is the focus of HHS.