I've been a hospitalist now for ten years. In those ten years I have continued to use a manual process for capturing patient billing information during daily rounds. These cards contain all the information necessary to generate payment claims from Medicare and other third party insurance companies. Over the years the cards have changed to add or remove elements required to receive payments and stay in compliance with third party payers. These cards fit nicely into our scrubs or white coat pockets.
I know many organizations have moved to real time submission of daily rounding charges to their billing company. I have seen a few smart phone applications out there that allow physicians to provide bedside charge capture with immediate transmission to their billing company or staff. In addition, some EHR products provide algorithms that provide physicians with the correct CPT code and electronic transmission of the charges in real time. This software and the fees that come with them can be quite expensive. As a group, we have continued to use our billing and coding cards as a manual physician data entry process that is scanned to the billing company for claims processing.
In my five years at The Happy Hospitalist, realized I have never given the general public a sense of how complex every single patient encounter is from the insurance side of daily hospitalist rounds. I'm not talking about how to choose the correct CPT® code to submit for each and every patient encounter. That's an entirely different topic for discussion. For that I created a bedside E/M reference card to help me stay in compliance with complex CMS billing rules.
I wrote this article to show the public how complex the business side of medicine is for every single encounter we generate and how we have chosen to organize all the necessary elements of a daily encounter, including CPT® codes, ICD codes and the PQRS elements. We created these cards in house. Through trial and error, we have found a layout for our daily charge capture card that works with great efficiency and accuracy.
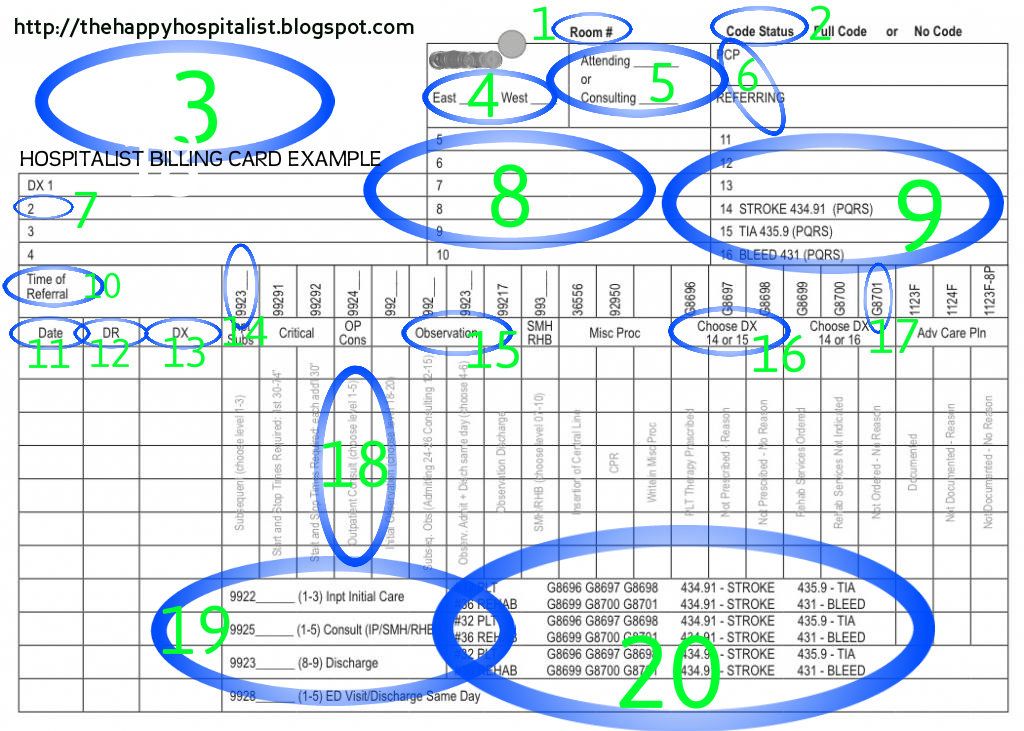
Many physicians who don't do their own charge capturing do not appreciate how complex this process is. I have provided below our most updated daily rounding charge capture cards currently in use for 2013. Each component is described below. This is the present state of American medicine. Physicians must comply with this process thousands of times a year with every patient encounter to get paid for the work they have provided. The first card is the side scanned to our billing company on every patient. The second picture is the backside of the card used only as a reference for physicians to determine the correct information to submit. See, you didn't just get a $90 out-of-pocket high deductible copay from doctor to tell you there is no treatment for you cold. You got a $10 opinion and an $80 bill to pay for all this madness.
I know many organizations have moved to real time submission of daily rounding charges to their billing company. I have seen a few smart phone applications out there that allow physicians to provide bedside charge capture with immediate transmission to their billing company or staff. In addition, some EHR products provide algorithms that provide physicians with the correct CPT code and electronic transmission of the charges in real time. This software and the fees that come with them can be quite expensive. As a group, we have continued to use our billing and coding cards as a manual physician data entry process that is scanned to the billing company for claims processing.
In my five years at The Happy Hospitalist, realized I have never given the general public a sense of how complex every single patient encounter is from the insurance side of daily hospitalist rounds. I'm not talking about how to choose the correct CPT® code to submit for each and every patient encounter. That's an entirely different topic for discussion. For that I created a bedside E/M reference card to help me stay in compliance with complex CMS billing rules.
I wrote this article to show the public how complex the business side of medicine is for every single encounter we generate and how we have chosen to organize all the necessary elements of a daily encounter, including CPT® codes, ICD codes and the PQRS elements. We created these cards in house. Through trial and error, we have found a layout for our daily charge capture card that works with great efficiency and accuracy.
Many physicians who don't do their own charge capturing do not appreciate how complex this process is. I have provided below our most updated daily rounding charge capture cards currently in use for 2013. Each component is described below. This is the present state of American medicine. Physicians must comply with this process thousands of times a year with every patient encounter to get paid for the work they have provided. The first card is the side scanned to our billing company on every patient. The second picture is the backside of the card used only as a reference for physicians to determine the correct information to submit. See, you didn't just get a $90 out-of-pocket high deductible copay from doctor to tell you there is no treatment for you cold. You got a $10 opinion and an $80 bill to pay for all this madness.
- Room number. Where is the patient at? This information is not necessary for getting paid, but can be helpful for our colleagues at times. Most of the time though, we'll use our hospital generated patient census to find you.
- Code status. Do you want to be resuscitated in case your heart stops? Again, this information is not mandatory but is helpful to know if all heck breaks loose. Many hospitals have no hospital wide standard for capturing accurate information for the patient record.
- Patient information. This is were we place our patient sticker with that contains the patient's name, hospital ID numbers and date of birth necessary to submit payment to third parties.
- Site of service. I work at two hospitals. This information lets us and the billing company know which hospital this service was provided at.
- Attending or consultant. This information is helpful to know whether we are required to provide the discharge summary. The discharge summary is provided by the attending physician or their representative. I don't know what effect this has on getting paid.
- PCP and referring physicians. We use this information to internally track who our referring physicians. This information is also helpful to know who to contact on discharge when patients leave the hospital and whom we should send our discharge summary.
- Diagnosis. We have 13 lines to provide our diagnoses. These are the ICD codes. It's a free-for-all here. Most physicians have never been trained in ICD coding, including me. I'm sure 90% of my codes make no sense, forcing some coding person is trying to decipher what I write to the nearest applicable ICD code. I can't wait for ICD-10.
- More lines for diagnosis. Yes, sometimes we fill all the lines, and more.
- PQRS ICD codes. These are the ICD codes we have chosen for our PQRS program. There aren't a lot of PQRS measures applicable to hospitalist medicine, but we have found these ICD codes capture the intent of our PQRS process. In 2015, if physicians have chosen not to participate in PQRS, they will be penalized 1.5% of all Medicare charges. This penalty will be based on 2013 PQRS data. These ICD codes are linked to the CPT codes in line 13, when applicable, to remain in compliance with PQRS requirements.
- Time of referral. We use this information to understand the busiest times of day for new encounters. Medicare does not pay more for a 2 am admission, but your plumber will. This is helpful for creating staffing solutions for our hospitalist program.
- Date of service. This information is mandatory for generating claims.
- Doctor providing service. This information is mandatory for generating claims. We use a number system to define the doctor. It's much shorter than writing out all the names. We hand over our cards to other doctors when we go off service so there may be more than one doctor with billing information on one card. We trust each other not to lose the cards or change our billing information.
- Diagnosis for that visit. This is where we write the number of the diagnosis (#7,8) to link the ICD code to our CPT code (#14). These are mandatory for claims submission. I usually pick the four most important ICD codes for my visit and write them here, even though I may manage 18 different issues during an encounter. We don't get paid based on how many ICD codes we write and I believe Medicare carriers only allow up to four ICD codes to be submitted during the claims process.
- CPT code number. All these numbers here are the CPT codes us doctors choose that we believe accurately reflects the level of service we have provided and that our documentation supports. The CPT code determines how much the doctor gets paid for that day's visit. It is the most important part of the whole card. Physicians should learn how to choose the correct code every time. This code is mandatory for claims submission.
- CPT code description. These are the general descriptive categories of our CPT codes.
- PQRS explanation. Here, we are attempting to help the physician define which ICD code to use with which PQRS G code. PQRS codes only apply to certain ICD codes. Certain PQRS codes only apply to certain CPT codes. Got it? Yeah, us too.
- PQRS G codes. This is the actual code we need to choose for our visit. Just pick one for each PQRS measure. Got it? Make sure you pick the right one!
- CPT options. Here we attempt to describe what the options are for our CPT codes (#14). Please pick the correct code doctor. We don't want you being accused of fraud.
- Admit/Consult/Discharge codes. We have elected to pull out these CPT codes from the above madness to allow more clarity for us and our billing company. As you can see, these codes require all the same elements of our daily rounding. But remember, Medicare does not recognize consult codes anymore. I know, it's too complicated.
- PQRS for admit/consult/discharge codes. This is self explanatory.
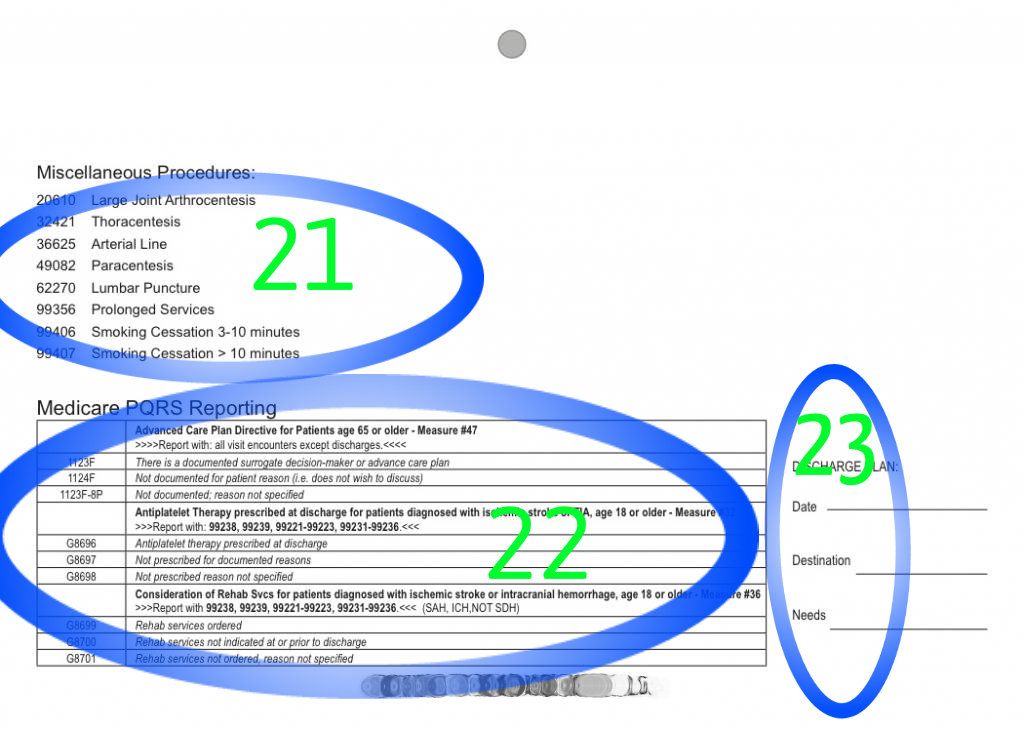
- CPT codes for additional procedures. We use this as reference for the CPT codes of additional procedures we may provide that aren't listed on the front of our cards. There just isn't room for everything!
- In depth PQRS descriptions. For our reference to decide which correct PQRS code is required.
- I have no idea what this is.
Any questions?

Tweet
Tidak ada komentar:
Posting Komentar